Tuesday Poster Session
Category: Colon
P3148 - Not Every Rectal Cancer Is Adenocarcinoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PS
Pranay Siriya, MD
Maimonides Medical Center
Brooklyn, New York
Presenting Author(s)
Syed Mujtaba Baqir, MBBS1, Avleen Kaur, MBBS1, Tiffany Lu, DO1, Neha Sharma, MD2, Aarti Maharaj, MBBS1, Pranay Siriya, MD1, Omair Khan, MBBS1, Meredith E. Pittman, MD1, Kelash Kumar, MD1, Kseniya Slobodyanyuk, MD3
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Health, Brooklyn, NY; 3Maimonides Medical Center, New York, NY
Introduction: The clinical spectrum of melanoma as a malignant anorectal cancer is infrequent, accounting for less than 1% of all melanomas and 0.25-1.25% of all anorectal cancers. However, it is a considerable diagnostic challenge owing to non-specific symptoms and hence misdiagnosis and histological discrepancies – the melanin pigment may not be prominent. We present the case of an elderly female who was admitted to the hospital due to several weeks of constipation, and that was posthumously discovered to be secondary to rectal melanoma.
Case Description/Methods: A 70-year-old woman with a history of hypertension, deep vein thrombosis, atrial fibrillation, and diabetes mellitus presented to the hospital for worsening constipation with associated rectal pain, bloating, and blood-streaked stools. Her family noted she was also progressively confused and lethargic compared to her baseline. She had been taking significant amounts of over-the-counter laxatives to have any bowel movements. Physical examination was notable for jaundice, a distended non-tender abdomen, and a palpable semi-circumferential lesion on digital rectal exam. CT scan of the abdomen and pelvis revealed small volume abdominal ascites heterogeneous liver with innumerable liver masses compatible with metastatic disease. Colonoscopy revealed a large rectal mass with 10-20mm polyps throughout the sigmoid colon and hepatic flexure. Multiple biopsies demonstrated sheets of cells with hyperchromatic nuclei, prominent nucleoli, and scant cytoplasm expressing SOX-10 and Melan-A with focal S-100 and CD117, consistent with malignant melanoma. Tumor marker levels demonstrated elevated CA19-9 290.3 U/mL (nl 0-35 U/mL) and normal CEA 1.5 ng/mL (0.3-2.5 ng/mL) and AFP 4.2 ng/mL (< 8.3ng/mL). Over the course of her hospitalization, the patient developed septic shock requiring vasopressors and broad-spectrum antibiotics. Given her poor prognosis, the patient’s surrogate decision-makers elected to initiate comfort care measures, and soon after, the patient passed.
Discussion: Anorectal malignant melanoma is a sporadic but very aggressive disease. It spreads along submucosal planes, and complete resection cannot be performed by the time of diagnosis. Patients typically succumb to complications of metastasis. Due to non-specific symptoms and poor prognosis at diagnosis, clinicians must keep rectal melanoma in the list of differentials in patients presenting with perirectal pain and hematochezia and not anchor to diagnosis such as hemorrhoids.

Disclosures:
Syed Mujtaba Baqir, MBBS1, Avleen Kaur, MBBS1, Tiffany Lu, DO1, Neha Sharma, MD2, Aarti Maharaj, MBBS1, Pranay Siriya, MD1, Omair Khan, MBBS1, Meredith E. Pittman, MD1, Kelash Kumar, MD1, Kseniya Slobodyanyuk, MD3. P3148 - Not Every Rectal Cancer Is Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Health, Brooklyn, NY; 3Maimonides Medical Center, New York, NY
Introduction: The clinical spectrum of melanoma as a malignant anorectal cancer is infrequent, accounting for less than 1% of all melanomas and 0.25-1.25% of all anorectal cancers. However, it is a considerable diagnostic challenge owing to non-specific symptoms and hence misdiagnosis and histological discrepancies – the melanin pigment may not be prominent. We present the case of an elderly female who was admitted to the hospital due to several weeks of constipation, and that was posthumously discovered to be secondary to rectal melanoma.
Case Description/Methods: A 70-year-old woman with a history of hypertension, deep vein thrombosis, atrial fibrillation, and diabetes mellitus presented to the hospital for worsening constipation with associated rectal pain, bloating, and blood-streaked stools. Her family noted she was also progressively confused and lethargic compared to her baseline. She had been taking significant amounts of over-the-counter laxatives to have any bowel movements. Physical examination was notable for jaundice, a distended non-tender abdomen, and a palpable semi-circumferential lesion on digital rectal exam. CT scan of the abdomen and pelvis revealed small volume abdominal ascites heterogeneous liver with innumerable liver masses compatible with metastatic disease. Colonoscopy revealed a large rectal mass with 10-20mm polyps throughout the sigmoid colon and hepatic flexure. Multiple biopsies demonstrated sheets of cells with hyperchromatic nuclei, prominent nucleoli, and scant cytoplasm expressing SOX-10 and Melan-A with focal S-100 and CD117, consistent with malignant melanoma. Tumor marker levels demonstrated elevated CA19-9 290.3 U/mL (nl 0-35 U/mL) and normal CEA 1.5 ng/mL (0.3-2.5 ng/mL) and AFP 4.2 ng/mL (< 8.3ng/mL). Over the course of her hospitalization, the patient developed septic shock requiring vasopressors and broad-spectrum antibiotics. Given her poor prognosis, the patient’s surrogate decision-makers elected to initiate comfort care measures, and soon after, the patient passed.
Discussion: Anorectal malignant melanoma is a sporadic but very aggressive disease. It spreads along submucosal planes, and complete resection cannot be performed by the time of diagnosis. Patients typically succumb to complications of metastasis. Due to non-specific symptoms and poor prognosis at diagnosis, clinicians must keep rectal melanoma in the list of differentials in patients presenting with perirectal pain and hematochezia and not anchor to diagnosis such as hemorrhoids.

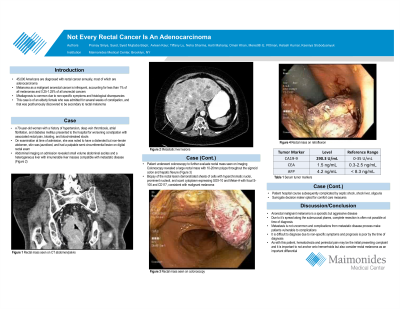
Figure: A: Semi circumferential rectal mass 2cm to 8cm from anal verge seen on forward view. The mass involved 50% of the circumference of the rectum
B: Multiple metastatic liver masses
B: Multiple metastatic liver masses
Disclosures:
Syed Mujtaba Baqir indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Tiffany Lu indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Aarti Maharaj indicated no relevant financial relationships.
Pranay Siriya indicated no relevant financial relationships.
Omair Khan indicated no relevant financial relationships.
Meredith Pittman indicated no relevant financial relationships.
Kelash Kumar indicated no relevant financial relationships.
Kseniya Slobodyanyuk indicated no relevant financial relationships.
Syed Mujtaba Baqir, MBBS1, Avleen Kaur, MBBS1, Tiffany Lu, DO1, Neha Sharma, MD2, Aarti Maharaj, MBBS1, Pranay Siriya, MD1, Omair Khan, MBBS1, Meredith E. Pittman, MD1, Kelash Kumar, MD1, Kseniya Slobodyanyuk, MD3. P3148 - Not Every Rectal Cancer Is Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
