Tuesday Poster Session
Category: Small Intestine
P4157 - Connecting the Dots: A Case of CMV Enteritis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Priyadarshini Loganathan, MD
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Mahesh Gajendran, MD, MPH1, Sadia Aslam, MD2, Priyadarshini Loganathan, MD3, Randy Wright, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: CMV is an opportunistic infection in immunocompromised patients and causes enteritis or colitis. The occurrence of CMV enteritis is rare in immunocompetent individuals, but sporadic cases have been reported in the literature.
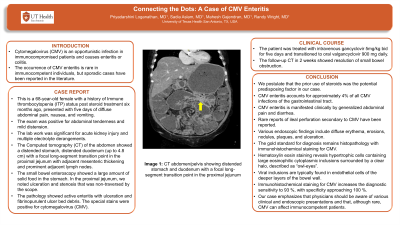
Case Description/Methods: This is a 68-year-old female with a history of Immune thrombocytopenia (ITP) status post steroid treatment 6 months ago, presented with five days of diffuse abdominal pain, nausea, and vomiting. The exam was positive for abdominal tenderness and mild distension. The lab work was significant for acute kidney injury and multiple electrolyte derangements. The Computed tomography (CT) of the abdomen showed distended stomach, distended duodenum (up to 4.8 cm) with a focal long-segment transition point in the proximal jejunum with adjacent mesenteric thickening and prominent adjacent lymph nodes. The small bowel enteroscopy showed a large amount of solid food in the stomach. In the proximal jejunum, a significant amount of solid food due to ulceration and stenosis that was non-traversed by the scope. The pathology showed active enteritis with ulceration and fibrinopurulent ulcer bed debris. The special stains were positive for cytomegalovirus (CMV). The patient was treated with intravenous gancyclovir 5mg/kg bid for five days and transitioned to oral valgancyclovir 900 mg daily. The follow-up CT in 2 weeks showed resolution of small bowel obstruction
Discussion: We postulate that the prior use of steroids was the potential predisposing factor in our case. CMV enteritis accounts for approximately 4% of all CMV infections of the gastrointestinal tract. CMV enteritis is manifested clinically by generalized abdominal pain and diarrhea. Rare reports of ileal perforation secondary to CMV have been reported. Various endoscopic findings include diffuse erythema, erosions, nodules, plaques, and ulceration. The gold standard for diagnosis remains histopathology with immunohistochemical staining for CMV. Hematoxylin eosin staining reveals hypertrophic cells containing large eosinophilic cytoplasmic inclusions surrounded by a clear halo, described as “owl-eyes”. Viral inclusions are typically found in endothelial cells of the deeper layers of the bowel wall. Immunohistochemical staining for CMV increases the diagnostic sensitivity to 93 %, with specificity approaching 100 %. Our case emphasizes that
physicians should be aware of various clinical and endoscopic presentations and that, although rare, CMV can affect immunocompetent patients.

Disclosures:
Mahesh Gajendran, MD, MPH1, Sadia Aslam, MD2, Priyadarshini Loganathan, MD3, Randy Wright, MD1. P4157 - Connecting the Dots: A Case of CMV Enteritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: CMV is an opportunistic infection in immunocompromised patients and causes enteritis or colitis. The occurrence of CMV enteritis is rare in immunocompetent individuals, but sporadic cases have been reported in the literature.
Case Description/Methods: This is a 68-year-old female with a history of Immune thrombocytopenia (ITP) status post steroid treatment 6 months ago, presented with five days of diffuse abdominal pain, nausea, and vomiting. The exam was positive for abdominal tenderness and mild distension. The lab work was significant for acute kidney injury and multiple electrolyte derangements. The Computed tomography (CT) of the abdomen showed distended stomach, distended duodenum (up to 4.8 cm) with a focal long-segment transition point in the proximal jejunum with adjacent mesenteric thickening and prominent adjacent lymph nodes. The small bowel enteroscopy showed a large amount of solid food in the stomach. In the proximal jejunum, a significant amount of solid food due to ulceration and stenosis that was non-traversed by the scope. The pathology showed active enteritis with ulceration and fibrinopurulent ulcer bed debris. The special stains were positive for cytomegalovirus (CMV). The patient was treated with intravenous gancyclovir 5mg/kg bid for five days and transitioned to oral valgancyclovir 900 mg daily. The follow-up CT in 2 weeks showed resolution of small bowel obstruction
Discussion: We postulate that the prior use of steroids was the potential predisposing factor in our case. CMV enteritis accounts for approximately 4% of all CMV infections of the gastrointestinal tract. CMV enteritis is manifested clinically by generalized abdominal pain and diarrhea. Rare reports of ileal perforation secondary to CMV have been reported. Various endoscopic findings include diffuse erythema, erosions, nodules, plaques, and ulceration. The gold standard for diagnosis remains histopathology with immunohistochemical staining for CMV. Hematoxylin eosin staining reveals hypertrophic cells containing large eosinophilic cytoplasmic inclusions surrounded by a clear halo, described as “owl-eyes”. Viral inclusions are typically found in endothelial cells of the deeper layers of the bowel wall. Immunohistochemical staining for CMV increases the diagnostic sensitivity to 93 %, with specificity approaching 100 %. Our case emphasizes that
physicians should be aware of various clinical and endoscopic presentations and that, although rare, CMV can affect immunocompetent patients.

Figure: Figure 1A: Computed tomography (CT) of the abdomen showed distended stomach, distended duodenum (up to 4.8 cm) with a focal long-segment transition point in the proximal jejunum with adjacent mesenteric thickening and prominent adjacent lymph nodes
Figure 1B and C: The small bowel enteroscopy showed a significant amount of solid food due to ulceration and stenosis that was non-traversed by the scope in the proximal jejunum
Figure 1D: High power field showing many inflammatory cells (mostly histiocytes plus neutrophils) and one large cell with “cytomegaly” which is a viral effect but no definite viral inclusions. The special stains were positive for cytomegalovirus (not included in this figure)
Figure 1B and C: The small bowel enteroscopy showed a significant amount of solid food due to ulceration and stenosis that was non-traversed by the scope in the proximal jejunum
Figure 1D: High power field showing many inflammatory cells (mostly histiocytes plus neutrophils) and one large cell with “cytomegaly” which is a viral effect but no definite viral inclusions. The special stains were positive for cytomegalovirus (not included in this figure)
Disclosures:
Mahesh Gajendran indicated no relevant financial relationships.
Sadia Aslam indicated no relevant financial relationships.
Priyadarshini Loganathan indicated no relevant financial relationships.
Randy Wright indicated no relevant financial relationships.
Mahesh Gajendran, MD, MPH1, Sadia Aslam, MD2, Priyadarshini Loganathan, MD3, Randy Wright, MD1. P4157 - Connecting the Dots: A Case of CMV Enteritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
