Tuesday Poster Session
Category: Colon
P3164 - A Case of Tuberculous Pseudomembranous Colitis With Associated Pseudoobstruction
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Briette Karanfilian, MD
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Briette Karanfilian, MD, Mahmoud Ali, MBBCh, Samuel Pan, BS, Anish V. Patel, MD
Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Pseudomembranous colitis (PC) is most commonly associated with clostridioides difficile (CD) infection, however, there are many other related entities, such as inflammatory bowel disease, ischemia, and other infections. There are very few reported cases of tuberculosis causing PC. To the best of our knowledge, this is the only case of a patient with tuberculous PC and colonic pseudoobstruction.
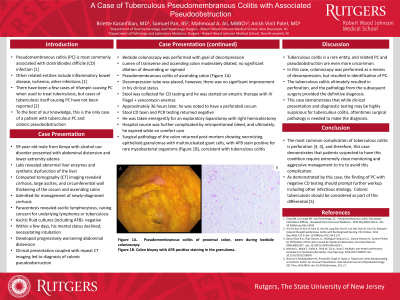
Case Description/Methods: A 59-year-old male from Kenya with alcohol use disorder presented with abdominal distension and lower extremity edema. Labs revealed abnormal liver enzymes and synthetic dysfunction of the liver. Computed tomography imaging revealed cirrhosis, large ascites, and circumferential wall thickening of the cecum and ascending colon. The patient was admitted for management of newly-diagnosed cirrhosis. Paracentesis revealed ascitic lymphocytosis, raising concern for underlying lymphoma or tuberculosis. Within a few days, his mental status declined, necessitating intubation. He developed progressively worsening abdominal distension and was diagnosed with colonic pseudoobstruction. Bedside colonoscopy was performed where the patient was found to have PC in the proximal colon (Figure 1A). Decompression tube was placed, however, there was no significant improvement in his clinical status, and approximately 36 hours later, he was noted to have a perforated cecum. Stool CD toxin and PCR testing returned negative. He was taken emergently for a right hemicolectomy. Hospital course was further complicated by retroperitoneal hemorrhage, and ultimately, he expired while on comfort care. Surgical pathology of the colon returned after he passed, showing necrotizing epithelioid granulomas with multinucleated giant cells, with AFB stain positive for rare mycobacterial organisms (Figure 1B), consistent with tuberculous colitis.
Discussion: Tuberculous colitis is a rare entity, and related PC is even more uncommon. This case demonstrates that while clinical presentation and diagnostic testing may be highly suspicious for this diagnosis, oftentimes surgical pathology is needed to make the diagnosis. The most common complication of tuberculous colitis is perforation, and therefore, this case demonstrates that patients suspected to have this condition require extremely close monitoring and aggressive management to try to avoid this complication. Additionally, as demonstrated by our case, the finding of PC with negative CD testing should prompt further workup, including other infectious etiology.

Disclosures:
Briette Karanfilian, MD, Mahmoud Ali, MBBCh, Samuel Pan, BS, Anish V. Patel, MD. P3164 - A Case of Tuberculous Pseudomembranous Colitis With Associated Pseudoobstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Pseudomembranous colitis (PC) is most commonly associated with clostridioides difficile (CD) infection, however, there are many other related entities, such as inflammatory bowel disease, ischemia, and other infections. There are very few reported cases of tuberculosis causing PC. To the best of our knowledge, this is the only case of a patient with tuberculous PC and colonic pseudoobstruction.
Case Description/Methods: A 59-year-old male from Kenya with alcohol use disorder presented with abdominal distension and lower extremity edema. Labs revealed abnormal liver enzymes and synthetic dysfunction of the liver. Computed tomography imaging revealed cirrhosis, large ascites, and circumferential wall thickening of the cecum and ascending colon. The patient was admitted for management of newly-diagnosed cirrhosis. Paracentesis revealed ascitic lymphocytosis, raising concern for underlying lymphoma or tuberculosis. Within a few days, his mental status declined, necessitating intubation. He developed progressively worsening abdominal distension and was diagnosed with colonic pseudoobstruction. Bedside colonoscopy was performed where the patient was found to have PC in the proximal colon (Figure 1A). Decompression tube was placed, however, there was no significant improvement in his clinical status, and approximately 36 hours later, he was noted to have a perforated cecum. Stool CD toxin and PCR testing returned negative. He was taken emergently for a right hemicolectomy. Hospital course was further complicated by retroperitoneal hemorrhage, and ultimately, he expired while on comfort care. Surgical pathology of the colon returned after he passed, showing necrotizing epithelioid granulomas with multinucleated giant cells, with AFB stain positive for rare mycobacterial organisms (Figure 1B), consistent with tuberculous colitis.
Discussion: Tuberculous colitis is a rare entity, and related PC is even more uncommon. This case demonstrates that while clinical presentation and diagnostic testing may be highly suspicious for this diagnosis, oftentimes surgical pathology is needed to make the diagnosis. The most common complication of tuberculous colitis is perforation, and therefore, this case demonstrates that patients suspected to have this condition require extremely close monitoring and aggressive management to try to avoid this complication. Additionally, as demonstrated by our case, the finding of PC with negative CD testing should prompt further workup, including other infectious etiology.

Figure: Figure 1A. Endoscopic image demonstrating pseudomembranous colitis. Figure 1B. Surgical pathology from hemicolectomy with acid-fast bacilli (AFB) positive staining in granulomas.
Disclosures:
Briette Karanfilian indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Samuel Pan indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Briette Karanfilian, MD, Mahmoud Ali, MBBCh, Samuel Pan, BS, Anish V. Patel, MD. P3164 - A Case of Tuberculous Pseudomembranous Colitis With Associated Pseudoobstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
