Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3186 - Factors Associated With Non-Completion of Mailed Fecal Immunohistochemical Tests
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Naveena Sunkara, MD
Warren Alpert Medical School, Brown University
Providence, RI
Presenting Author(s)
Naveena Sunkara, MD1, Tyler Selig, MD2, Yousef Elfanagely, MD2, Sohum A. Patwa, MD2, Kathryn Evey, DO3, Kittichai Promrat, MD4
1Warren Alpert Medical School, Brown University, Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Warren Alpert School of Medicine at Brown University, Providence, RI; 4Brown University, Providence, RI
Introduction: The COVID-19 pandemic led to a sharp decrease in colorectal cancer screening rates as all non-urgent procedures, including average-risk screening colonoscopies, were suspended for infection control and resource conservation. In response to pandemic restrictions, we pivoted to a mailed Fecal Immunohistochemical Tests (FIT) outreach initiative. Here we examine factors and patient characteristics that influenced rates of completion and areas for targeted outreach improvement.
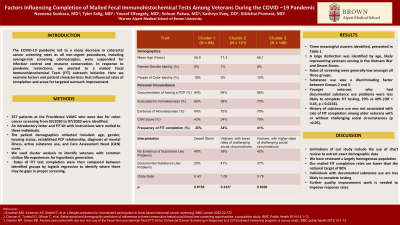
Methods: A total of 357 patients at the Providence VA Medical Center who were due for colon cancer screening from 03/2020 to 07/2020 were identified. An introductory letter and FIT kit with instructions were mailed to these individuals. The patient demographics collected included: age, gender, housing status, established PCP relationship, diagnosis of mental illness, active substance use, and Care Assessment Need (CAN) score. We used cluster analysis to identify veterans with common civilian life experiences for hypothesis generation. Rates of FIT test completion were then compared between identified groups by logistic regression to identify where there may be gaps in proper screening.
Results: We identified three meaningful clusters, presented in Table 1. A large distinction was identified by age, likely representing veterans serving in the Vietnam War and Desert Storm. There was a correspondence between substance use and other social circumstances (i.e., mental health problems, homelessness). We focused on comparing veterans demonstrating substance use problems to those that did not, as an operationalization of broader problems with civilian life. Younger veterans who had documented substance use problems were less likely to complete FIT testing, 29% vs 49% (OR = 0.43, p = 0.0156). However, history of substance use was not associated with rate of FIT completion among older veterans with or without challenging social circumstances (p >0.05).
Discussion: Our primary conclusion is that older veterans (Cluster 2 and 3) did not demonstrate a difference in FIT testing completion rates regardless of their social circumstances. Younger veterans however, demonstrated that completion of FIT testing varied with their social circumstances. Those with documented substance use were less likely to complete testing. This finding will be important in designing larger mailed FIT program targeting younger veterans.
Disclosures:
Naveena Sunkara, MD1, Tyler Selig, MD2, Yousef Elfanagely, MD2, Sohum A. Patwa, MD2, Kathryn Evey, DO3, Kittichai Promrat, MD4. P3186 - Factors Associated With Non-Completion of Mailed Fecal Immunohistochemical Tests, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Warren Alpert Medical School, Brown University, Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Warren Alpert School of Medicine at Brown University, Providence, RI; 4Brown University, Providence, RI
Introduction: The COVID-19 pandemic led to a sharp decrease in colorectal cancer screening rates as all non-urgent procedures, including average-risk screening colonoscopies, were suspended for infection control and resource conservation. In response to pandemic restrictions, we pivoted to a mailed Fecal Immunohistochemical Tests (FIT) outreach initiative. Here we examine factors and patient characteristics that influenced rates of completion and areas for targeted outreach improvement.
Methods: A total of 357 patients at the Providence VA Medical Center who were due for colon cancer screening from 03/2020 to 07/2020 were identified. An introductory letter and FIT kit with instructions were mailed to these individuals. The patient demographics collected included: age, gender, housing status, established PCP relationship, diagnosis of mental illness, active substance use, and Care Assessment Need (CAN) score. We used cluster analysis to identify veterans with common civilian life experiences for hypothesis generation. Rates of FIT test completion were then compared between identified groups by logistic regression to identify where there may be gaps in proper screening.
Results: We identified three meaningful clusters, presented in Table 1. A large distinction was identified by age, likely representing veterans serving in the Vietnam War and Desert Storm. There was a correspondence between substance use and other social circumstances (i.e., mental health problems, homelessness). We focused on comparing veterans demonstrating substance use problems to those that did not, as an operationalization of broader problems with civilian life. Younger veterans who had documented substance use problems were less likely to complete FIT testing, 29% vs 49% (OR = 0.43, p = 0.0156). However, history of substance use was not associated with rate of FIT completion among older veterans with or without challenging social circumstances (p >0.05).
Discussion: Our primary conclusion is that older veterans (Cluster 2 and 3) did not demonstrate a difference in FIT testing completion rates regardless of their social circumstances. Younger veterans however, demonstrated that completion of FIT testing varied with their social circumstances. Those with documented substance use were less likely to complete testing. This finding will be important in designing larger mailed FIT program targeting younger veterans.
Disclosures:
Naveena Sunkara indicated no relevant financial relationships.
Tyler Selig indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Sohum Patwa indicated no relevant financial relationships.
Kathryn Evey indicated no relevant financial relationships.
Kittichai Promrat indicated no relevant financial relationships.
Naveena Sunkara, MD1, Tyler Selig, MD2, Yousef Elfanagely, MD2, Sohum A. Patwa, MD2, Kathryn Evey, DO3, Kittichai Promrat, MD4. P3186 - Factors Associated With Non-Completion of Mailed Fecal Immunohistochemical Tests, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
