Tuesday Poster Session
Category: Stomach
P4187 - The Interplay of Celiac Sprue and Use of ARBs in the Development of Collagenous Gastritis: A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- NA
Nicole Anastasio, DO
University of Connecticut School of Medicine
Farmington, CT
Presenting Author(s)
Nicole Anastasio, DO1, Teresa Da Cunha, MD1, Lisa Rossi, MD2
1University of Connecticut School of Medicine, Farmington, CT; 2Saint Francis Hospital-Trinity Health of New England, Hartford, CT
Introduction: Collagenous gastritis (CG) is a rare condition of unknown etiology characterized by increased deposition of collagen ( > 10μm) in the subepithelial layer of the stomach with accompanying inflammatory infiltration. The pathogenesis of CG largely remains unclear. However, several autoimmune diseases and certain medications have been implicated as triggers for its development. The case herein describes the interplay of autoimmune disease and the use of ARBs as predisposing risk factors.
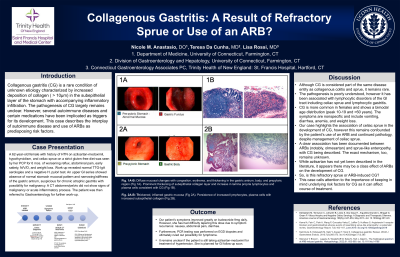
Case Description/Methods: A 62-year-old female with history of HTN on azilsartan, hypothyroidism, and celiac sprue on a strict gluten-free diet was seen by her PCP for 6 mos. of worsening reflux, abdominal pain, early satiety, N/V/D, and weight loss. Work-up revealed normal TTG-IgA serologies and a negative H. pylori test. An upper GI series showed absence of normal stomach mucosal pattern and narrowing/stiffness of the gastric antrum, suspicious for chronic atrophic gastritis with possibility for malignancy. A CT abdomen/pelvis did not show signs of malignancy or acute inflammatory process. Subsequently, an EGD revealed diffuse mucosal changes with congestion, erythema, and thickening in the gastric antrum, body, and prepyloric region. The examined duodenum was normal. The pathology report showed prominent thickening of subepithelial collagen layer and increase in lamina propria lymphocytes and plasma cells consistent with CG. She was trialed on PPI with no improvement in symptoms and transitioned to budesonide with resolution of her symptoms.
Discussion: Although CG is considered part of the same disease entity as collagenous colitis and sprue, it remains rare. The pathogenesis is poorly understood but has been associated with lymphocytic disorders of the GI tract including celiac sprue and lymphocytic gastritis. It is more common in females and shows a bimodal age distribution (peak 10-19 and >60 years). The symptoms are nonspecific and include diarrhea, anemia, vomiting, and weight loss. Our case highlights the association of celiac sprue with CG.
Additionally, a clear association has been documented between ARBs (notably, olmesartan) and sprue-like enteropathy, with CG also being described; nonetheless the exact mechanism remains unknown. Despite strict dietary adherence, our patient developed CG calling into question the role of azilsartan in its development, an ARB not yet described in the literature.
This case helps gastroenterologists to be mindful when faced by patients with underlying risk factors for CG.
Disclosures:
Nicole Anastasio, DO1, Teresa Da Cunha, MD1, Lisa Rossi, MD2. P4187 - The Interplay of Celiac Sprue and Use of ARBs in the Development of Collagenous Gastritis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Connecticut School of Medicine, Farmington, CT; 2Saint Francis Hospital-Trinity Health of New England, Hartford, CT
Introduction: Collagenous gastritis (CG) is a rare condition of unknown etiology characterized by increased deposition of collagen ( > 10μm) in the subepithelial layer of the stomach with accompanying inflammatory infiltration. The pathogenesis of CG largely remains unclear. However, several autoimmune diseases and certain medications have been implicated as triggers for its development. The case herein describes the interplay of autoimmune disease and the use of ARBs as predisposing risk factors.
Case Description/Methods: A 62-year-old female with history of HTN on azilsartan, hypothyroidism, and celiac sprue on a strict gluten-free diet was seen by her PCP for 6 mos. of worsening reflux, abdominal pain, early satiety, N/V/D, and weight loss. Work-up revealed normal TTG-IgA serologies and a negative H. pylori test. An upper GI series showed absence of normal stomach mucosal pattern and narrowing/stiffness of the gastric antrum, suspicious for chronic atrophic gastritis with possibility for malignancy. A CT abdomen/pelvis did not show signs of malignancy or acute inflammatory process. Subsequently, an EGD revealed diffuse mucosal changes with congestion, erythema, and thickening in the gastric antrum, body, and prepyloric region. The examined duodenum was normal. The pathology report showed prominent thickening of subepithelial collagen layer and increase in lamina propria lymphocytes and plasma cells consistent with CG. She was trialed on PPI with no improvement in symptoms and transitioned to budesonide with resolution of her symptoms.
Discussion: Although CG is considered part of the same disease entity as collagenous colitis and sprue, it remains rare. The pathogenesis is poorly understood but has been associated with lymphocytic disorders of the GI tract including celiac sprue and lymphocytic gastritis. It is more common in females and shows a bimodal age distribution (peak 10-19 and >60 years). The symptoms are nonspecific and include diarrhea, anemia, vomiting, and weight loss. Our case highlights the association of celiac sprue with CG.
Additionally, a clear association has been documented between ARBs (notably, olmesartan) and sprue-like enteropathy, with CG also being described; nonetheless the exact mechanism remains unknown. Despite strict dietary adherence, our patient developed CG calling into question the role of azilsartan in its development, an ARB not yet described in the literature.
This case helps gastroenterologists to be mindful when faced by patients with underlying risk factors for CG.
Disclosures:
Nicole Anastasio indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Lisa Rossi indicated no relevant financial relationships.
Nicole Anastasio, DO1, Teresa Da Cunha, MD1, Lisa Rossi, MD2. P4187 - The Interplay of Celiac Sprue and Use of ARBs in the Development of Collagenous Gastritis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
