Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3196 - Effect of Artificial Intelligence Polyp Detection in an Office-Based Endoscopy Practice
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- TD
Timothy R. Dougherty, Jr., MD
Digestive Disease Physicians
Alexandria, VA
Presenting Author(s)
Alexander C. Ellison, 1, Chloe E. Dougherty, 2, Pavit S. George, 3, Tahlia G. Conway, 4, Sophia G.. Dougherty, 2, Lyna Atiyeh, MD5, Wendy M.. Shaw, MS, BSN, RN5, Timothy R.. Dougherty, MD5
1Flint Hill School, Oakton, VA; 2James Madison High School, Vienna, VA; 3St. Albans School, Washington, DC; 4Georgetown Visitation Preparatory School, Washington, DC; 5Digestive Disease Physicians, Alexandria, VA
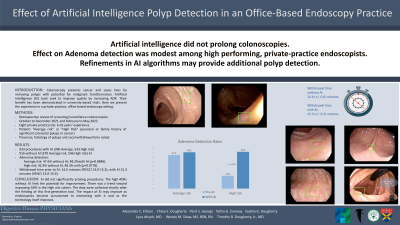
Introduction: Colonoscopy prevents cancer and saves lives by removing polyps with potential for malignant transformation. Increasing Adenoma Detection Rate (ADR) decreases the risk for missed lesions and interval cancers. Gastroenterologists have sought to increase the impact of colonoscopy by improving quality and increasing the ADR. Prior efforts focused on technique, e.g., optimizing cecum withdrawal times and laxative preparation. Artificial Intelligence (AI) tools seek to further improve colonoscopy quality by increasing ADR. Their benefit has been demonstrated in university-based trials. Here we present the experience in a private-practice, office-based endoscopy setting.
Methods: This retrospective review examined screening/surveillance colonoscopies performed for patients over 45 years old. Colonoscopy reports from October to December 2021 and February to May 2022 were examined. Colonoscopies were performed by eight private practice, fellowship-trained gastroenterologists with 6-35 years’ experience. Patients were deemed “Average risk” or “High Risk” with the latter defined as a personal or family history of significant colorectal polyps or cancer. Diagnostic exams were excluded. The presence and histology of polyps and the cecal withdrawal time were noted. Categorical variables were examined using Fischer’s Exact Test and 95% confidence intervals calculated for numerical variables.
Results: There were 933 procedures assisted with GI Genius (Medtronic, Minneapolis, MN) including 390 Average risk patients and 543 High risk. Another 370 Average risk and 546 High risk colonoscopies without AI were examined. Among the Average risk, 176 patients (47.6%) examined without AI had adenomas detected as did 188 (48.2%) of those examined with AI (p=0.8846). There were 234 patients (42.9%) at High risk with adenomas detected. Another 262 (48.3%) had adenomas detected using AI (p=0.0778). The mean withdrawal time prior to fielding AI was 14.6 minutes (95%CI 14.0-15.2) and with AI was 15.3 minutes (95%CI 15.0-15.6).
Discussion: This review showed the use AI did not significantly prolong procedures. The group’s high ADRs without AI limits the potential for improvement. There was a trend toward improving ADR, particularly in the High risk cohort. The data were collected shortly after the fielding of this first-generation tool. The impact of AI may improve as endoscopists become accustomed to interacting with it and as the technology itself improves.
Disclosures:
Alexander C. Ellison, 1, Chloe E. Dougherty, 2, Pavit S. George, 3, Tahlia G. Conway, 4, Sophia G.. Dougherty, 2, Lyna Atiyeh, MD5, Wendy M.. Shaw, MS, BSN, RN5, Timothy R.. Dougherty, MD5. P3196 - Effect of Artificial Intelligence Polyp Detection in an Office-Based Endoscopy Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Flint Hill School, Oakton, VA; 2James Madison High School, Vienna, VA; 3St. Albans School, Washington, DC; 4Georgetown Visitation Preparatory School, Washington, DC; 5Digestive Disease Physicians, Alexandria, VA
Introduction: Colonoscopy prevents cancer and saves lives by removing polyps with potential for malignant transformation. Increasing Adenoma Detection Rate (ADR) decreases the risk for missed lesions and interval cancers. Gastroenterologists have sought to increase the impact of colonoscopy by improving quality and increasing the ADR. Prior efforts focused on technique, e.g., optimizing cecum withdrawal times and laxative preparation. Artificial Intelligence (AI) tools seek to further improve colonoscopy quality by increasing ADR. Their benefit has been demonstrated in university-based trials. Here we present the experience in a private-practice, office-based endoscopy setting.
Methods: This retrospective review examined screening/surveillance colonoscopies performed for patients over 45 years old. Colonoscopy reports from October to December 2021 and February to May 2022 were examined. Colonoscopies were performed by eight private practice, fellowship-trained gastroenterologists with 6-35 years’ experience. Patients were deemed “Average risk” or “High Risk” with the latter defined as a personal or family history of significant colorectal polyps or cancer. Diagnostic exams were excluded. The presence and histology of polyps and the cecal withdrawal time were noted. Categorical variables were examined using Fischer’s Exact Test and 95% confidence intervals calculated for numerical variables.
Results: There were 933 procedures assisted with GI Genius (Medtronic, Minneapolis, MN) including 390 Average risk patients and 543 High risk. Another 370 Average risk and 546 High risk colonoscopies without AI were examined. Among the Average risk, 176 patients (47.6%) examined without AI had adenomas detected as did 188 (48.2%) of those examined with AI (p=0.8846). There were 234 patients (42.9%) at High risk with adenomas detected. Another 262 (48.3%) had adenomas detected using AI (p=0.0778). The mean withdrawal time prior to fielding AI was 14.6 minutes (95%CI 14.0-15.2) and with AI was 15.3 minutes (95%CI 15.0-15.6).
Discussion: This review showed the use AI did not significantly prolong procedures. The group’s high ADRs without AI limits the potential for improvement. There was a trend toward improving ADR, particularly in the High risk cohort. The data were collected shortly after the fielding of this first-generation tool. The impact of AI may improve as endoscopists become accustomed to interacting with it and as the technology itself improves.
Disclosures:
Alexander Ellison indicated no relevant financial relationships.
Chloe Dougherty indicated no relevant financial relationships.
Pavit George indicated no relevant financial relationships.
Tahlia Conway indicated no relevant financial relationships.
Sophia Dougherty indicated no relevant financial relationships.
Lyna Atiyeh indicated no relevant financial relationships.
Wendy Shaw indicated no relevant financial relationships.
Timothy Dougherty indicated no relevant financial relationships.
Alexander C. Ellison, 1, Chloe E. Dougherty, 2, Pavit S. George, 3, Tahlia G. Conway, 4, Sophia G.. Dougherty, 2, Lyna Atiyeh, MD5, Wendy M.. Shaw, MS, BSN, RN5, Timothy R.. Dougherty, MD5. P3196 - Effect of Artificial Intelligence Polyp Detection in an Office-Based Endoscopy Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
