Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3199 - Impact of Artificial Intelligence on Colorectal Adenoma Detection in High-Risk Colonoscopy: Initial Experience at a Safety-Net Hospital
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kenneth Chow, MD
Harbor-UCLA Medical Center
Torrance, CA
Presenting Author(s)
Kenneth Chow, MD, Matthew Bell, MD, Maryanne Amour, MD, Viktor Eysselein, MD, Neetika Srivastava, MD, Michael Wayne Fleischman, MD, Sofiya Reicher, MD
Harbor-UCLA Medical Center, Torrance, CA
Introduction: Increased adenoma detection rates (ADR) have recently been demonstrated in artificial intelligence (AI)-assisted colonoscopies. However, the data on the “real world” performance of AI and its effect on polyp detection is quite limited. We analyzed the AI impact in a diverse patient population undergoing diagnostic colonoscopy for positive colorectal cancer (CRC) screening tests or symptoms.
Methods: We reviewed colonoscopies performed from August 1, 2022 to April 30, 2023. In our safety net resource-limited healthcare system, fecal immunochemical testing (FIT) is the preferred CRC screening strategy, with colonoscopies reserved for diagnostic indications: history of adenomas, CRC family history, bleeding, iron-deficiency anemia, or positive FIT. AI software (GI Genius, Medtronic) was incorporated into the standard procedure protocol in November 2022. Polyp detection metrics were reviewed in 3 time periods: pre-AI (8/1/2022 to 10/31/2022), early post-AI (12/1/2022 to 2/28/2023), and established post-AI (3/1/2023 to 4/30/2023). Two separate timepoints were used post AI implementation to account for initial learning curve. All colonoscopies were performed by or under the supervision of endoscopists with significant ( >3000 colonoscopies) experience; “second look” examination or retroflexion was routinely performed in the right colon. Data was collected on patient demographics, procedure indication, polyp size, location, and pathology.
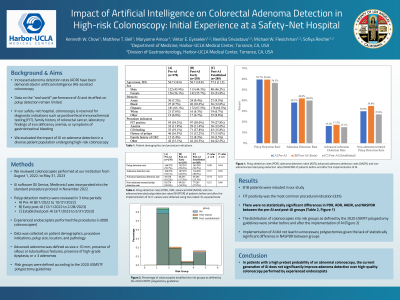
Results: In total, 706 patients were analyzed: 278 patients in the pre-AI group, 255 patients in the post-AI (early) group, and 173 patients in the post-AI (established) group. The most common procedural indication was FIT positivity. The polyp detection rate (PDR) was 59.7% in the pre-AI group, 59.6% in the post-AI (early) group (p=0.98), and 58.4% in the post-AI (established) group (p=0.78). The adenoma detection rate (ADR) was 38.1% in the pre-AI group, 42.0% in the post-AI (early) group (p=0.37), and 41.5% in the post-AI (established) group (p=0.46). [Figure] In the post-AI (early) group, 23.1% of patients had at least one non-adenoma/serrated polyp and 17.3% in the pre-AI group (p=0.21). [Table]
Discussion: In our experience, there were no significant differences in PDR or ADR in the pre-AI versus post-AI-groups. Our findings suggest that in patients with increased pre-test probability of an abnormal colonoscopy, current generation AI software does not significantly improve ADRs over high-quality colonoscopy performed by experienced endoscopists.

Disclosures:
Kenneth Chow, MD, Matthew Bell, MD, Maryanne Amour, MD, Viktor Eysselein, MD, Neetika Srivastava, MD, Michael Wayne Fleischman, MD, Sofiya Reicher, MD. P3199 - Impact of Artificial Intelligence on Colorectal Adenoma Detection in High-Risk Colonoscopy: Initial Experience at a Safety-Net Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Harbor-UCLA Medical Center, Torrance, CA
Introduction: Increased adenoma detection rates (ADR) have recently been demonstrated in artificial intelligence (AI)-assisted colonoscopies. However, the data on the “real world” performance of AI and its effect on polyp detection is quite limited. We analyzed the AI impact in a diverse patient population undergoing diagnostic colonoscopy for positive colorectal cancer (CRC) screening tests or symptoms.
Methods: We reviewed colonoscopies performed from August 1, 2022 to April 30, 2023. In our safety net resource-limited healthcare system, fecal immunochemical testing (FIT) is the preferred CRC screening strategy, with colonoscopies reserved for diagnostic indications: history of adenomas, CRC family history, bleeding, iron-deficiency anemia, or positive FIT. AI software (GI Genius, Medtronic) was incorporated into the standard procedure protocol in November 2022. Polyp detection metrics were reviewed in 3 time periods: pre-AI (8/1/2022 to 10/31/2022), early post-AI (12/1/2022 to 2/28/2023), and established post-AI (3/1/2023 to 4/30/2023). Two separate timepoints were used post AI implementation to account for initial learning curve. All colonoscopies were performed by or under the supervision of endoscopists with significant ( >3000 colonoscopies) experience; “second look” examination or retroflexion was routinely performed in the right colon. Data was collected on patient demographics, procedure indication, polyp size, location, and pathology.
Results: In total, 706 patients were analyzed: 278 patients in the pre-AI group, 255 patients in the post-AI (early) group, and 173 patients in the post-AI (established) group. The most common procedural indication was FIT positivity. The polyp detection rate (PDR) was 59.7% in the pre-AI group, 59.6% in the post-AI (early) group (p=0.98), and 58.4% in the post-AI (established) group (p=0.78). The adenoma detection rate (ADR) was 38.1% in the pre-AI group, 42.0% in the post-AI (early) group (p=0.37), and 41.5% in the post-AI (established) group (p=0.46). [Figure] In the post-AI (early) group, 23.1% of patients had at least one non-adenoma/serrated polyp and 17.3% in the pre-AI group (p=0.21). [Table]
Discussion: In our experience, there were no significant differences in PDR or ADR in the pre-AI versus post-AI-groups. Our findings suggest that in patients with increased pre-test probability of an abnormal colonoscopy, current generation AI software does not significantly improve ADRs over high-quality colonoscopy performed by experienced endoscopists.

Figure: Polyp detection rate, adenoma detection rate, and non-adenoma/serrated polyp detection rates before and after the implementation of AI.
Disclosures:
Kenneth Chow indicated no relevant financial relationships.
Matthew Bell indicated no relevant financial relationships.
Maryanne Amour indicated no relevant financial relationships.
Viktor Eysselein indicated no relevant financial relationships.
Neetika Srivastava indicated no relevant financial relationships.
Michael Wayne Fleischman indicated no relevant financial relationships.
Sofiya Reicher: Boston Scientific – Consultant.
Kenneth Chow, MD, Matthew Bell, MD, Maryanne Amour, MD, Viktor Eysselein, MD, Neetika Srivastava, MD, Michael Wayne Fleischman, MD, Sofiya Reicher, MD. P3199 - Impact of Artificial Intelligence on Colorectal Adenoma Detection in High-Risk Colonoscopy: Initial Experience at a Safety-Net Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
