Tuesday Poster Session
Category: Stomach
P4222 - Ischemic Gastritis Due to Mycotic Embolism in the Setting of Group B Strep Bacteremia: A Fatally Rare Case
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Bryant Pinto Javier, DO, MHA
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Bryant Pinto. Javier, DO, MHA, Rajiv Singh, MD, Uday Patel, DO, Mohammed Mustafa. Hasan, MD, Christopher Calcagno, DO
Parkview Medical Center, Pueblo, CO
Introduction: Gastric ischemia is rare due to the extensive collateral blood supply to the stomach. However, vascular insufficiency caused by hypotension, vasculitis, or, as we present here, disseminated septic embolism can lead to gastric ischemia.
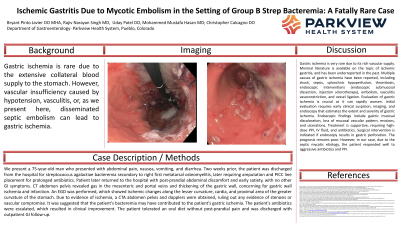
Case Description/Methods: We present a 75-year-old man who presented with abdominal pain, nausea, vomiting, and diarrhea. Two weeks prior, the patient was discharged from the hospital for streptococcus agalactiae bacteremia secondary to right first metatarsal osteomyelitis, later requiring amputation and PICC line placement for prolonged antibiotics. Patient later returned to the hospital with post-prandial abdominal discomfort and early satiety, with no other GI symptoms. CT abdomen pelvis revealed gas in the mesenteric and portal veins and thickening of the gastric wall, concerning for gastric wall ischemia and infarction. An EGD was performed, which showed ischemic changes along the lesser curvature, cardia, and proximal area of the greater curvature of the stomach. Due to evidence of ischemia, a CTA abdomen pelvis and dopplers were obtained, ruling out any evidence of stenosis or vascular compromise. It was suggested that the patient's bacteremia may have contributed to the patient's gastric ischemia. The patient's antibiotics were escalated, which resulted in clinical improvement. The patient tolerated an oral diet without post-prandial pain and was discharged with outpatient GI follow-up.
Discussion: Gastric ischemia is very rare due to its rich vascular supply. Minimal literature is available on the topic of ischemic gastritis, and has been underreported in the past. Multiple causes of gastric ischemia have been reported, including shock, sepsis, splanchnic hypoperfusion, thrombosis, endoscopic interventions (endoscopic submucosal dissection, injection sclerotherapy), embolism, vasculitis vasoconstriction, and vessel ligation. Evaluation of gastric ischemia is crucial as it can rapidly worsen. Initial evaluation requires early clinical suspicion, imaging, and endoscopy that estimates the extent and severity of gastric ischemia. Endoscopic findings include gastric mucosal discoloration, loss of mucosal vascular pattern, erosions, and ulcerations. Treatment is supportive, requiring high-dose PPI, IV fluid, and antibiotics. Surgical intervention is indicated if endoscopy results in gastric perforation. The prognosis remains poor. However, in our case, due to the septic mycotic etiology, the patient responded well to aggressive antibiotics and PPI.

Disclosures:
Bryant Pinto. Javier, DO, MHA, Rajiv Singh, MD, Uday Patel, DO, Mohammed Mustafa. Hasan, MD, Christopher Calcagno, DO. P4222 - Ischemic Gastritis Due to Mycotic Embolism in the Setting of Group B Strep Bacteremia: A Fatally Rare Case, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Parkview Medical Center, Pueblo, CO
Introduction: Gastric ischemia is rare due to the extensive collateral blood supply to the stomach. However, vascular insufficiency caused by hypotension, vasculitis, or, as we present here, disseminated septic embolism can lead to gastric ischemia.
Case Description/Methods: We present a 75-year-old man who presented with abdominal pain, nausea, vomiting, and diarrhea. Two weeks prior, the patient was discharged from the hospital for streptococcus agalactiae bacteremia secondary to right first metatarsal osteomyelitis, later requiring amputation and PICC line placement for prolonged antibiotics. Patient later returned to the hospital with post-prandial abdominal discomfort and early satiety, with no other GI symptoms. CT abdomen pelvis revealed gas in the mesenteric and portal veins and thickening of the gastric wall, concerning for gastric wall ischemia and infarction. An EGD was performed, which showed ischemic changes along the lesser curvature, cardia, and proximal area of the greater curvature of the stomach. Due to evidence of ischemia, a CTA abdomen pelvis and dopplers were obtained, ruling out any evidence of stenosis or vascular compromise. It was suggested that the patient's bacteremia may have contributed to the patient's gastric ischemia. The patient's antibiotics were escalated, which resulted in clinical improvement. The patient tolerated an oral diet without post-prandial pain and was discharged with outpatient GI follow-up.
Discussion: Gastric ischemia is very rare due to its rich vascular supply. Minimal literature is available on the topic of ischemic gastritis, and has been underreported in the past. Multiple causes of gastric ischemia have been reported, including shock, sepsis, splanchnic hypoperfusion, thrombosis, endoscopic interventions (endoscopic submucosal dissection, injection sclerotherapy), embolism, vasculitis vasoconstriction, and vessel ligation. Evaluation of gastric ischemia is crucial as it can rapidly worsen. Initial evaluation requires early clinical suspicion, imaging, and endoscopy that estimates the extent and severity of gastric ischemia. Endoscopic findings include gastric mucosal discoloration, loss of mucosal vascular pattern, erosions, and ulcerations. Treatment is supportive, requiring high-dose PPI, IV fluid, and antibiotics. Surgical intervention is indicated if endoscopy results in gastric perforation. The prognosis remains poor. However, in our case, due to the septic mycotic etiology, the patient responded well to aggressive antibiotics and PPI.

Figure: Gastric wall ischemia visualized on EGD
Disclosures:
Bryant Javier indicated no relevant financial relationships.
Rajiv Singh indicated no relevant financial relationships.
Uday Patel indicated no relevant financial relationships.
Mohammed Hasan indicated no relevant financial relationships.
Christopher Calcagno indicated no relevant financial relationships.
Bryant Pinto. Javier, DO, MHA, Rajiv Singh, MD, Uday Patel, DO, Mohammed Mustafa. Hasan, MD, Christopher Calcagno, DO. P4222 - Ischemic Gastritis Due to Mycotic Embolism in the Setting of Group B Strep Bacteremia: A Fatally Rare Case, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
