Tuesday Poster Session
Category: Stomach
P4223 - Acquired Double Pylorus: A Rare Endoscopic Finding of Severe Peptic Ulcer Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Laura Miranda, MD
Broward Health North
Deerfield Beach, FL
Presenting Author(s)
Laura Miranda, MD, Kristina Nemeth, MD, John Rivas, MD
Broward Health North, Deerfield Beach, FL
Introduction: Double pylorus (DP) is a rare condition that may occur as a congenital gastrointestinal duplication abnormality or, more commonly, as an acquired complication of a penetrating ulcer due to gastric malignancy or peptic ulcer disease. It is characterized by a gastroduodenal fistula (GDF) extending from the gastric antrum into the duodenal bulb. It is a rare endoscopic finding, seen in less than 0.4% of upper GI endoscopies. We report a case of endoscopically-diagnosed ADP in a female with severe peptic ulcer disease secondary to chronic NSAID use.
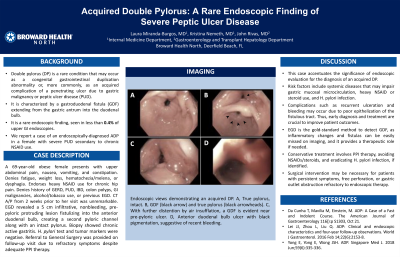
Case Description/Methods: A 69-year-old obese female presents with upper abdominal pain, nausea, vomiting, and constipation. Denies fatigue, weight loss, hematochezia/melena, or dysphagia. She endorses heavy NSAID use for chronic hip pain. Denies history of GERD, PUD, IBD, colon polyps, GI malignancies, alcohol/tobacco use, or previous EGD. Abdominal CT from 2 weeks prior to her visit was unremarkable. EGD revealed a 5 cm infiltrative, nonbleeding, pre-pyloric protruding lesion fistulizing into the anterior duodenal bulb, creating a second pyloric channel along with an intact pylorus. Biopsy showed chronic active gastritis. Helicobacter pylori test and tumor markers were negative. Referral to General Surgery was provided on follow-up visit due to refractory symptoms despite adequate PPI therapy.
Discussion: This case accentuates the significance of endoscopic evaluation for the diagnosis of an acquired DP as a result of peptic ulcer disease. Risk factors include systemic diseases that may impair gastric mucosal microcirculation, heavy NSAID or steroid use, and H. pylori infection. Complications such as recurrent ulceration and bleeding may occur due to poor epithelization of the fistulous tract. Thus, early diagnosis and treatment are crucial to improve patient outcomes. EGD is the gold-standard method to detect GDF, as inflammatory changes and fistulas can be easily missed on contrast-enhanced imaging, and it provides a therapeutic role if needed. Conservative treatment involves PPI therapy, avoiding NSAIDs/steroids, and eradicating H. pylori infection, if identified. Surgical intervention may be necessary for patients with persistent symptoms, free perforation, or gastric outlet obstruction refractory to endoscopic therapy.

Disclosures:
Laura Miranda, MD, Kristina Nemeth, MD, John Rivas, MD. P4223 - Acquired Double Pylorus: A Rare Endoscopic Finding of Severe Peptic Ulcer Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Broward Health North, Deerfield Beach, FL
Introduction: Double pylorus (DP) is a rare condition that may occur as a congenital gastrointestinal duplication abnormality or, more commonly, as an acquired complication of a penetrating ulcer due to gastric malignancy or peptic ulcer disease. It is characterized by a gastroduodenal fistula (GDF) extending from the gastric antrum into the duodenal bulb. It is a rare endoscopic finding, seen in less than 0.4% of upper GI endoscopies. We report a case of endoscopically-diagnosed ADP in a female with severe peptic ulcer disease secondary to chronic NSAID use.
Case Description/Methods: A 69-year-old obese female presents with upper abdominal pain, nausea, vomiting, and constipation. Denies fatigue, weight loss, hematochezia/melena, or dysphagia. She endorses heavy NSAID use for chronic hip pain. Denies history of GERD, PUD, IBD, colon polyps, GI malignancies, alcohol/tobacco use, or previous EGD. Abdominal CT from 2 weeks prior to her visit was unremarkable. EGD revealed a 5 cm infiltrative, nonbleeding, pre-pyloric protruding lesion fistulizing into the anterior duodenal bulb, creating a second pyloric channel along with an intact pylorus. Biopsy showed chronic active gastritis. Helicobacter pylori test and tumor markers were negative. Referral to General Surgery was provided on follow-up visit due to refractory symptoms despite adequate PPI therapy.
Discussion: This case accentuates the significance of endoscopic evaluation for the diagnosis of an acquired DP as a result of peptic ulcer disease. Risk factors include systemic diseases that may impair gastric mucosal microcirculation, heavy NSAID or steroid use, and H. pylori infection. Complications such as recurrent ulceration and bleeding may occur due to poor epithelization of the fistulous tract. Thus, early diagnosis and treatment are crucial to improve patient outcomes. EGD is the gold-standard method to detect GDF, as inflammatory changes and fistulas can be easily missed on contrast-enhanced imaging, and it provides a therapeutic role if needed. Conservative treatment involves PPI therapy, avoiding NSAIDs/steroids, and eradicating H. pylori infection, if identified. Surgical intervention may be necessary for patients with persistent symptoms, free perforation, or gastric outlet obstruction refractory to endoscopic therapy.

Figure: Endoscopic views demonstrating an acquired DP. A, True pylorus, intact. B, GDF (black arrow) and true pylorus (black arrowheads). C, With further distention by air insufflation, a GDF is evident near pre-pyloric ulcer. D, Anterior duodenal bulb ulcer with black pigmentation, suggestive of recent bleeding.
Disclosures:
Laura Miranda indicated no relevant financial relationships.
Kristina Nemeth indicated no relevant financial relationships.
John Rivas indicated no relevant financial relationships.
Laura Miranda, MD, Kristina Nemeth, MD, John Rivas, MD. P4223 - Acquired Double Pylorus: A Rare Endoscopic Finding of Severe Peptic Ulcer Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

