Tuesday Poster Session
Category: Esophagus
P3239 - Tooting Its Horn: Nasal Trumpet Improves Success of High-Resolution Esophageal Manometry Catheter Placement
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Angela Wu, MD
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Angela Wu, MD, Andrew Leopold, MD, Guofeng Xie, MBBS, PhD
University of Maryland School of Medicine, Baltimore, MD
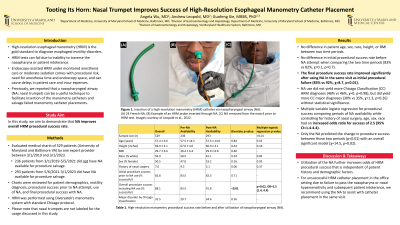
Introduction: High-resolution esophageal manometry (HRM) is the gold standard for diagnosing esophageal motility disorders. However, HRM tests can fail due to inability to traverse the nares or patient intolerance. Previously, we reported that a nasopharyngeal airway (NA; nasal trumpet) can be a useful technique to facilitate insertion of the manometry catheters. In this study, we aim to demonstrate that NA improves overall HRM procedure success rate.
Methods: Patients at two institutions who underwent HRM by one expert provider between 3/1/2019 and 3/1/2023 were evaluated. Charts were reviewed for patient demographics, motility diagnosis, procedural success prior to NA attempt, use of NA, and final procedural success with NA. Patients from 3/1/2019-5/5/2021 who did not have NA available for procedure salvage were compared to patients from 5/6/2021-3/1/2023 who had NA available. HRM was performed using Diversatek’s manometry system with standard Chicago protocol.
Results: 529 HRM studies were conducted; 236 occurred prior to NA availability, and 293 occurred after NA was utilized. There was no difference in patient age, sex, race, height, or BMI between those two periods.
There was no difference in initial procedural success rate before NA attempt when comparing the period prior to NA availability to the period with NA availability (83% vs 82%, χ=0.1, p=0.7). After using NA in cases of initial procedural failure during the same visit, the final procedure success rate improved significantly (83% vs 92%, χ=8.7, p< 0.01). This did not yield more Chicago Classification (CC) HRM diagnoses (46% vs 46%, χ=0, p=0.98), but did yield more CC major diagnosis (30% vs 35%, χ=1.3, p=0.26) without statistical significance.
Multiple variable logistic regression for procedural success comparing periods of NA availability while controlling for history of nasal surgery, age, height, race, and sex had an improved odds ratio for success of 2.5 (95% CI=1.4-4.4). Only the NA predicted the change in procedure success between those two periods (p< 0.01) with an overall significant model (χ=14.5, p=0.02).
Discussion: Utilization of the NA further increases odds of HRM procedural success that is independent of patient history and demographic factors. For unsuccessful HRM catheter placement in the office setting due to failure to pass the nares or nasal hypersensitivity, we recommend using the NA to assist with catheter placement during the same visit.
Disclosures:
Angela Wu, MD, Andrew Leopold, MD, Guofeng Xie, MBBS, PhD. P3239 - Tooting Its Horn: Nasal Trumpet Improves Success of High-Resolution Esophageal Manometry Catheter Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Maryland School of Medicine, Baltimore, MD
Introduction: High-resolution esophageal manometry (HRM) is the gold standard for diagnosing esophageal motility disorders. However, HRM tests can fail due to inability to traverse the nares or patient intolerance. Previously, we reported that a nasopharyngeal airway (NA; nasal trumpet) can be a useful technique to facilitate insertion of the manometry catheters. In this study, we aim to demonstrate that NA improves overall HRM procedure success rate.
Methods: Patients at two institutions who underwent HRM by one expert provider between 3/1/2019 and 3/1/2023 were evaluated. Charts were reviewed for patient demographics, motility diagnosis, procedural success prior to NA attempt, use of NA, and final procedural success with NA. Patients from 3/1/2019-5/5/2021 who did not have NA available for procedure salvage were compared to patients from 5/6/2021-3/1/2023 who had NA available. HRM was performed using Diversatek’s manometry system with standard Chicago protocol.
Results: 529 HRM studies were conducted; 236 occurred prior to NA availability, and 293 occurred after NA was utilized. There was no difference in patient age, sex, race, height, or BMI between those two periods.
There was no difference in initial procedural success rate before NA attempt when comparing the period prior to NA availability to the period with NA availability (83% vs 82%, χ=0.1, p=0.7). After using NA in cases of initial procedural failure during the same visit, the final procedure success rate improved significantly (83% vs 92%, χ=8.7, p< 0.01). This did not yield more Chicago Classification (CC) HRM diagnoses (46% vs 46%, χ=0, p=0.98), but did yield more CC major diagnosis (30% vs 35%, χ=1.3, p=0.26) without statistical significance.
Multiple variable logistic regression for procedural success comparing periods of NA availability while controlling for history of nasal surgery, age, height, race, and sex had an improved odds ratio for success of 2.5 (95% CI=1.4-4.4). Only the NA predicted the change in procedure success between those two periods (p< 0.01) with an overall significant model (χ=14.5, p=0.02).
Discussion: Utilization of the NA further increases odds of HRM procedural success that is independent of patient history and demographic factors. For unsuccessful HRM catheter placement in the office setting due to failure to pass the nares or nasal hypersensitivity, we recommend using the NA to assist with catheter placement during the same visit.
Disclosures:
Angela Wu indicated no relevant financial relationships.
Andrew Leopold indicated no relevant financial relationships.
Guofeng Xie indicated no relevant financial relationships.
Angela Wu, MD, Andrew Leopold, MD, Guofeng Xie, MBBS, PhD. P3239 - Tooting Its Horn: Nasal Trumpet Improves Success of High-Resolution Esophageal Manometry Catheter Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
