Tuesday Poster Session
Category: Stomach
P4241 - A Diagnostic Dilemma of Gastric Submucosal Tumor
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Oliver Lee, DO
Tripler Army Medical Center
Honolulu, HI
Presenting Author(s)
Oliver Lee, DO, Emily Wickersham, DO, Ogle Jenie, MD, Pedro Manibusan, DO, MBA
Tripler Army Medical Center, Honolulu, HI
Introduction: Pancreatic heterotopia is a rare congenital anomaly, defined as pancreatic tissue separated from the main pancreatic gland without continuity of duct system or vascularity. The lesions are usually found within the stomach or proximal intestine but can occur throughout gastrointestinal tract; and rarely in extra-gastrointestinal sites. While most pancreatic heterotopia do not have clinical significance, some lesions may lead to inflammation, bleeding, obstruction, and in rare cases, malignant transformation, requiring surgical or endoscopic resection.
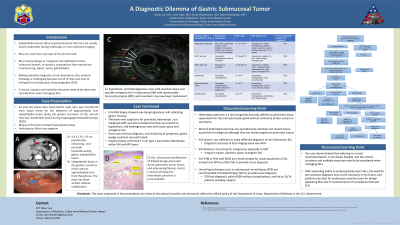
Case Description/Methods: We present a 42-year-old active-duty service member who was transferred from South Korea for evaluation of a 4.4 x 1.8 x 1.9 cm peripherally enhancing and centrally hypoattenuating ill-defined gastric submucosal tumor seen on contrast-enhanced CT. This mass was initially found during esophagogastroduodenoscopy (EGD) as part of work-up for chronic epigastric discomfort, early satiety, and bloating which was refractory to proton pump inhibitor. Biopsy showed hyperplastic polyp, and Helicobacter Pylori was negative. Upon arrival to the military treatment facility, repeat EGD showed a submucosal lesion >2cm in the gastric antrum without umbilicus. Radial endoscopic ultrasound (EUS) showed hypoechoic and heterogeneous mass with indistinct margins, including anechoic areas, in submucosa and muscularis propria layers with questionable deep mucosa layer involvement. These findings were suspicious for pancreatic heterotopia, but GIST was also considered as they can rarely present as heterogenous lesions with irregular margins and ulceration. Unfortunately, EUS-FNA biopsy showed only benign glandular cells indicating gastric mucosa. Given the lack of tissue diagnosis and chronicity of symptoms, gastric wedge resection was performed. Surgical biopsy confirmed 1.5 cm type 1 pancreatic heterotopia within the submucosa and muscularis propria layers.
Discussion: Making an accurate diagnosis for a gastric submucosal tumor is critical as misdiagnosis can be fatal. Despite having advanced diagnostic tools, the frequent inability to differentiate pancreatic heterotopia from malignancy often necessitates surgical excision in order to make the definitive diagnosis on histopathology.

Disclosures:
Oliver Lee, DO, Emily Wickersham, DO, Ogle Jenie, MD, Pedro Manibusan, DO, MBA. P4241 - A Diagnostic Dilemma of Gastric Submucosal Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Tripler Army Medical Center, Honolulu, HI
Introduction: Pancreatic heterotopia is a rare congenital anomaly, defined as pancreatic tissue separated from the main pancreatic gland without continuity of duct system or vascularity. The lesions are usually found within the stomach or proximal intestine but can occur throughout gastrointestinal tract; and rarely in extra-gastrointestinal sites. While most pancreatic heterotopia do not have clinical significance, some lesions may lead to inflammation, bleeding, obstruction, and in rare cases, malignant transformation, requiring surgical or endoscopic resection.
Case Description/Methods: We present a 42-year-old active-duty service member who was transferred from South Korea for evaluation of a 4.4 x 1.8 x 1.9 cm peripherally enhancing and centrally hypoattenuating ill-defined gastric submucosal tumor seen on contrast-enhanced CT. This mass was initially found during esophagogastroduodenoscopy (EGD) as part of work-up for chronic epigastric discomfort, early satiety, and bloating which was refractory to proton pump inhibitor. Biopsy showed hyperplastic polyp, and Helicobacter Pylori was negative. Upon arrival to the military treatment facility, repeat EGD showed a submucosal lesion >2cm in the gastric antrum without umbilicus. Radial endoscopic ultrasound (EUS) showed hypoechoic and heterogeneous mass with indistinct margins, including anechoic areas, in submucosa and muscularis propria layers with questionable deep mucosa layer involvement. These findings were suspicious for pancreatic heterotopia, but GIST was also considered as they can rarely present as heterogenous lesions with irregular margins and ulceration. Unfortunately, EUS-FNA biopsy showed only benign glandular cells indicating gastric mucosa. Given the lack of tissue diagnosis and chronicity of symptoms, gastric wedge resection was performed. Surgical biopsy confirmed 1.5 cm type 1 pancreatic heterotopia within the submucosa and muscularis propria layers.
Discussion: Making an accurate diagnosis for a gastric submucosal tumor is critical as misdiagnosis can be fatal. Despite having advanced diagnostic tools, the frequent inability to differentiate pancreatic heterotopia from malignancy often necessitates surgical excision in order to make the definitive diagnosis on histopathology.

Figure: Figure 1. A) Endoscopic Ultrasound showed a hypoechoic and heterogenous mass with anechoic areas in submucosa and muscularis propria layers with questionable deep mucosa layer involvement; B) Endoscopy showed ~2cm gastric submucosal tumor (SMT) covered with normal mucosa without umbilicus in gastric antrum; C) Contrast-enhanced CT showed a 1.8cm x 1.9cm peripherally enhancing and centrally hypoattenuating ill-defined gastric submucosal tumor
Disclosures:
Oliver Lee indicated no relevant financial relationships.
Emily Wickersham indicated no relevant financial relationships.
Ogle Jenie indicated no relevant financial relationships.
Pedro Manibusan indicated no relevant financial relationships.
Oliver Lee, DO, Emily Wickersham, DO, Ogle Jenie, MD, Pedro Manibusan, DO, MBA. P4241 - A Diagnostic Dilemma of Gastric Submucosal Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
