Tuesday Poster Session
Category: Esophagus
P3242 - Eosinophilic Esophagitis Is Significantly More Prevalent Among Whites Compared to Other Ethnic Groups: Are Genetics a Factor?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Collin Mayemura, MD
Keck School of Medicine of USC
Los Angeles, CA
Presenting Author(s)
Collin Mayemura, MD1, Nicholas Placone, MD1, Jennifer L. Dodge, MPH2, Denis Nguyen, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
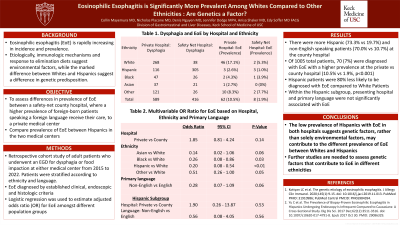
Introduction: Eosinophilic esophagitis (EoE) is rapidly increasing in incidence and prevalence. Etiologically, immunologic mechanisms and response to elimination diets suggest environmental factors, while the marked difference in prevalence between whites and Hispanics suggest a difference in genetic predisposition. We compare prevalence of EoE between a private medical center and a safety-net county hospital where a higher prevalence of foreign-born patients, using foreign language, receive their care. We hypothesize that a shorter sojourn in the community of the latter group can help elucidate a greater importance of genetics over environmental factors in EoE.
Methods: This is a retrospective cohort study of adult patients who underwent upper endoscopy for dysphagia or food impaction at two medical centers: private versus county from 2015 to 2022. The outcome of EoE was based on clinical and endoscopic presentation and the presence of proximal or distal esophageal biopsy showing ≥ 15 eosinophils per high power field not attributable to other diagnoses such as gastroesophageal reflux or achalasia. Logistic regression estimated adjusted odds ratio (OR) for EoE.
Results: Of 1004 patients, 58.7% presented to the private hospital, with more Hispanic (73.3% vs 19.7%) and non-English speaking patients (70.0% vs 10.7%) at the county hospital. EoE was diagnosed in 70 (7.0%) patients total, with higher prevalence at the private vs county hospital (10.5% vs 1.9%, p< 0.001). A similar by hospital trend was seen for white (17.2% vs 5.3%, p=0.06) but not Hispanic (2.6% vs 1.0%, p=0.35), Black (4.3% vs 3.8%, p=1.00), Asian (2.7% vs 0%, p=1.00) or other race (8.3% vs 7.7%, p=1.00). On multivariable analysis, odds of EoE were lower for Hispanic vs white patients (OR=0.20, 95% CI 0.08-0.54) and trended toward non-English primary language vs English (OR=0.28, 95% CI 0.07-1.09). Presenting hospital was not significant (P=0.14). In the Hispanic subgroup, hospital and primary language were not significantly associated with EoE.
Discussion: Hispanic patients were 80% less likely to be diagnosed with EoE compared to white patients. Non-English language and county hospital had a similar but not significant trend. These findings suggest that the environmental exposures of foreign-born patients are less of a factor while genetics may explain differences in prevalence, particularly the protective effect of Hispanic ethnicity. Further studies are needed to assess genetic factors that contribute to EoE in different ethnicities.
Disclosures:
Collin Mayemura, MD1, Nicholas Placone, MD1, Jennifer L. Dodge, MPH2, Denis Nguyen, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1. P3242 - Eosinophilic Esophagitis Is Significantly More Prevalent Among Whites Compared to Other Ethnic Groups: Are Genetics a Factor?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Eosinophilic esophagitis (EoE) is rapidly increasing in incidence and prevalence. Etiologically, immunologic mechanisms and response to elimination diets suggest environmental factors, while the marked difference in prevalence between whites and Hispanics suggest a difference in genetic predisposition. We compare prevalence of EoE between a private medical center and a safety-net county hospital where a higher prevalence of foreign-born patients, using foreign language, receive their care. We hypothesize that a shorter sojourn in the community of the latter group can help elucidate a greater importance of genetics over environmental factors in EoE.
Methods: This is a retrospective cohort study of adult patients who underwent upper endoscopy for dysphagia or food impaction at two medical centers: private versus county from 2015 to 2022. The outcome of EoE was based on clinical and endoscopic presentation and the presence of proximal or distal esophageal biopsy showing ≥ 15 eosinophils per high power field not attributable to other diagnoses such as gastroesophageal reflux or achalasia. Logistic regression estimated adjusted odds ratio (OR) for EoE.
Results: Of 1004 patients, 58.7% presented to the private hospital, with more Hispanic (73.3% vs 19.7%) and non-English speaking patients (70.0% vs 10.7%) at the county hospital. EoE was diagnosed in 70 (7.0%) patients total, with higher prevalence at the private vs county hospital (10.5% vs 1.9%, p< 0.001). A similar by hospital trend was seen for white (17.2% vs 5.3%, p=0.06) but not Hispanic (2.6% vs 1.0%, p=0.35), Black (4.3% vs 3.8%, p=1.00), Asian (2.7% vs 0%, p=1.00) or other race (8.3% vs 7.7%, p=1.00). On multivariable analysis, odds of EoE were lower for Hispanic vs white patients (OR=0.20, 95% CI 0.08-0.54) and trended toward non-English primary language vs English (OR=0.28, 95% CI 0.07-1.09). Presenting hospital was not significant (P=0.14). In the Hispanic subgroup, hospital and primary language were not significantly associated with EoE.
Discussion: Hispanic patients were 80% less likely to be diagnosed with EoE compared to white patients. Non-English language and county hospital had a similar but not significant trend. These findings suggest that the environmental exposures of foreign-born patients are less of a factor while genetics may explain differences in prevalence, particularly the protective effect of Hispanic ethnicity. Further studies are needed to assess genetic factors that contribute to EoE in different ethnicities.
Disclosures:
Collin Mayemura indicated no relevant financial relationships.
Nicholas Placone indicated no relevant financial relationships.
Jennifer Dodge indicated no relevant financial relationships.
Denis Nguyen indicated no relevant financial relationships.
Anisa Shaker indicated no relevant financial relationships.
Edy Soffer indicated no relevant financial relationships.
Collin Mayemura, MD1, Nicholas Placone, MD1, Jennifer L. Dodge, MPH2, Denis Nguyen, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1. P3242 - Eosinophilic Esophagitis Is Significantly More Prevalent Among Whites Compared to Other Ethnic Groups: Are Genetics a Factor?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
