Tuesday Poster Session
Category: Stomach
P4252 - Weight Loss as a Manifestation of Autoimmune Gastritis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RB
Raveena Boodram, MD
University of Miami Miller School of Medicine / Jackson Memorial Hospital
Mimai, Florida
Presenting Author(s)
Keri-Ann Buchanan-Peart, MD1, Sabrina Taldone, MD, MBA1, Rodrigo Santoscoy Valencia, MD1, Raveena Boodram, MD2, Jamie S. Barkin, MD, MACG3
1University of Miami Miller School of Medicine / Jackson Memorial Hospital, Miami, FL; 2University of Miami Miller School of Medicine / Jackson Memorial Hospital, Mimai, FL; 3University of Miami, Leonard M. Miller School of Medicine, Miami, FL
Introduction: Autoimmune gastritis (AIG) is a chronic inflammatory disease characterized by gradual destruction of parietal cells leading to hypochlorhydria and intrinsic factor deficiency. Due to malabsorption, these changes frequently cause micronutrient deficiencies such as vitamin B12 and iron, which typically account for patients’ symptoms at presentation. This case report aims to highlight that isolated weight loss can be the initial presentation of AIG.
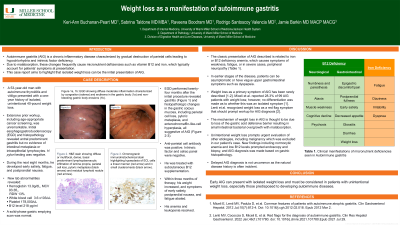
Case Description/Methods: A 53-year-old man with autoimmune thyroiditis and vitiligo presented with a one-year history of isolated, unintentional 40-pound weight loss. Extensive prior workup, including age-appropriate cancer screening, was unremarkable. Initial esophagogastroduodenoscopy (EGD) and histopathology revealed antral predominant gastritis and H. pylori testing negative. Weight loss was initially attributed to supratherapeutic levothyroxine therapy but despite achieving a euthyroid state, his weight continued to decline. During the next eight months, he developed early satiety, fatigue, and postprandial nausea. Lab abnormalities revealed hemoglobin 13.0g/dL (MCV 93.3fL, RDW 13%), WBC 3.6 x103/uL, platelet 178,000/uL, and B12 level 218 pg/ml. Solid-phase gastric emptying scan was normal. Repeat EGD, 24 months after the initial EGD, revealed gastritis (Figure 1) and histopathologic changes in the gastric corpus mucosa, including parietal cell loss, pyloric metaplasia, and enterochromaffin-like-cell hyperplasia, all suggestive of AIG. Anti-parietal cell antibody was positive. Intrinsic factor and celiac panel were negative. He was treated with B12 supplementation and within three months, his weight increased and symptoms abated.
Discussion: Classic AIG presentation is related to iron or B12 deficiency anemia (Table 1). Weight loss as a primary symptom of AIG has been rarely described. The mechanism is thought to be due to loss of the gastric acid defensive barrier resulting in small intestinal bacterial overgrowth with malabsorption. Unintentional weight loss prompts evaluation of many etiologies, but AIG is often not considered. Delayed diagnosis increases the risk of complications including gastric malignancy (gastric neuroendocrine tumor and adenocarcinoma). Early AIG can present with isolated weight loss and must be considered in patients with unintentional weight loss, especially those predisposed to developing autoimmune diseases.

Disclosures:
Keri-Ann Buchanan-Peart, MD1, Sabrina Taldone, MD, MBA1, Rodrigo Santoscoy Valencia, MD1, Raveena Boodram, MD2, Jamie S. Barkin, MD, MACG3. P4252 - Weight Loss as a Manifestation of Autoimmune Gastritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Miami Miller School of Medicine / Jackson Memorial Hospital, Miami, FL; 2University of Miami Miller School of Medicine / Jackson Memorial Hospital, Mimai, FL; 3University of Miami, Leonard M. Miller School of Medicine, Miami, FL
Introduction: Autoimmune gastritis (AIG) is a chronic inflammatory disease characterized by gradual destruction of parietal cells leading to hypochlorhydria and intrinsic factor deficiency. Due to malabsorption, these changes frequently cause micronutrient deficiencies such as vitamin B12 and iron, which typically account for patients’ symptoms at presentation. This case report aims to highlight that isolated weight loss can be the initial presentation of AIG.
Case Description/Methods: A 53-year-old man with autoimmune thyroiditis and vitiligo presented with a one-year history of isolated, unintentional 40-pound weight loss. Extensive prior workup, including age-appropriate cancer screening, was unremarkable. Initial esophagogastroduodenoscopy (EGD) and histopathology revealed antral predominant gastritis and H. pylori testing negative. Weight loss was initially attributed to supratherapeutic levothyroxine therapy but despite achieving a euthyroid state, his weight continued to decline. During the next eight months, he developed early satiety, fatigue, and postprandial nausea. Lab abnormalities revealed hemoglobin 13.0g/dL (MCV 93.3fL, RDW 13%), WBC 3.6 x103/uL, platelet 178,000/uL, and B12 level 218 pg/ml. Solid-phase gastric emptying scan was normal. Repeat EGD, 24 months after the initial EGD, revealed gastritis (Figure 1) and histopathologic changes in the gastric corpus mucosa, including parietal cell loss, pyloric metaplasia, and enterochromaffin-like-cell hyperplasia, all suggestive of AIG. Anti-parietal cell antibody was positive. Intrinsic factor and celiac panel were negative. He was treated with B12 supplementation and within three months, his weight increased and symptoms abated.
Discussion: Classic AIG presentation is related to iron or B12 deficiency anemia (Table 1). Weight loss as a primary symptom of AIG has been rarely described. The mechanism is thought to be due to loss of the gastric acid defensive barrier resulting in small intestinal bacterial overgrowth with malabsorption. Unintentional weight loss prompts evaluation of many etiologies, but AIG is often not considered. Delayed diagnosis increases the risk of complications including gastric malignancy (gastric neuroendocrine tumor and adenocarcinoma). Early AIG can present with isolated weight loss and must be considered in patients with unintentional weight loss, especially those predisposed to developing autoimmune diseases.

Figure: Figure 1a, 1b: EGD showing diffuse moderate inflammation characterized by congestion (edema) and erythema in the gastric body (1a) and non-bleeding gastric body erosions (1b).
Disclosures:
Keri-Ann Buchanan-Peart indicated no relevant financial relationships.
Sabrina Taldone indicated no relevant financial relationships.
Rodrigo Santoscoy Valencia indicated no relevant financial relationships.
Raveena Boodram indicated no relevant financial relationships.
Jamie Barkin indicated no relevant financial relationships.
Keri-Ann Buchanan-Peart, MD1, Sabrina Taldone, MD, MBA1, Rodrigo Santoscoy Valencia, MD1, Raveena Boodram, MD2, Jamie S. Barkin, MD, MACG3. P4252 - Weight Loss as a Manifestation of Autoimmune Gastritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
