Tuesday Poster Session
Category: Esophagus
P3252 - EGD Findings That Do No Not Explain Dysphagia Are Associated With Underutilization of High Resolution Manometry
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sydney Pomenti, MD
New York Presbyterian-Columbia
New York, NY
Presenting Author(s)
Sydney Pomenti, MD1, John Nathanson, MD2, Meaghan Phipps, MD1, Chino Aneke-Nash, MD, PhD1, David A.. Katzka, MD1, Daniel Freedberg, MD1, Daniela Jodorkovsky, MD3
1New York Presbyterian-Columbia, New York, NY; 2New York Prebyterian-Columbia, New York, NY; 3Mount Sinai, New York, NY
Introduction: In patients with dysphagia that is not explained by upper endoscopy, high-resolution esophageal manometry (HRM) is the next logical step in diagnostic testing. This study investigated predictors of failure to refer for HRM after an upper endoscopy that was performed for but did not explain dysphagia.
Methods: This was a retrospective cohort study of patients over 18 who underwent esophagogastroduodenoscopy (EGD) for dysphagia from 2015 to 2021. Patients with EGD findings that explained dysphagia (e.g., esophageal mass, eosinophilic esophagitis, Schatzki ring, etc) were excluded from the main analyses. The primary outcome was failure to refer for HRM within one year of the index non-diagnostic EGD. We also investigated delayed referral for HRM, defined as HRM performed after the median. Multivariable logistic regression modeling was used to identify risk factors which independently predicted failure to refer for HRM, conditioned on the providing endoscopist.
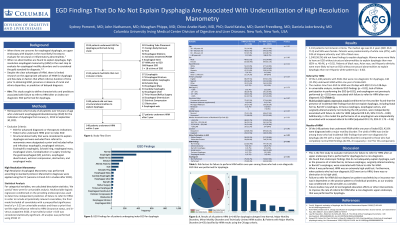
Results: Among 2,132 patients who underwent EGD for dysphagia, 1,240 (58.2%) did not have findings to explain dysphagia on the index EGD. Of these 1,240 patients, 148 (11.9%) underwent HRM within one year of index EGD. Endoscopic findings that did not explain dysphagia (e.g., hiatal hernia, tortuous esophagus, Barrett’s esophagus, altered anatomy) were independently associated with failure to refer for HRM (aOR 0.45, 95% CI 0.25 – 0.80). Demographic factors including race/ethnicity, insurance type, and income were not associated with failure to refer for HRM or delayed HRM. Of HRMs performed, 42.6% showed a major motility disorder and 6.8% showed a minor motility disorder. The diagnosis of a major motility disorder found on HRM was similar among those who had incidental EGD findings that were non-diagnostic for dysphagia compared to those who had completely normal EGD findings (42.4% vs. 42.6%, p = 0.27).
Discussion: Findings unrelated to dysphagia appear to deter providers from referring for HRM despite its high yield.

Disclosures:
Sydney Pomenti, MD1, John Nathanson, MD2, Meaghan Phipps, MD1, Chino Aneke-Nash, MD, PhD1, David A.. Katzka, MD1, Daniel Freedberg, MD1, Daniela Jodorkovsky, MD3. P3252 - EGD Findings That Do No Not Explain Dysphagia Are Associated With Underutilization of High Resolution Manometry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian-Columbia, New York, NY; 2New York Prebyterian-Columbia, New York, NY; 3Mount Sinai, New York, NY
Introduction: In patients with dysphagia that is not explained by upper endoscopy, high-resolution esophageal manometry (HRM) is the next logical step in diagnostic testing. This study investigated predictors of failure to refer for HRM after an upper endoscopy that was performed for but did not explain dysphagia.
Methods: This was a retrospective cohort study of patients over 18 who underwent esophagogastroduodenoscopy (EGD) for dysphagia from 2015 to 2021. Patients with EGD findings that explained dysphagia (e.g., esophageal mass, eosinophilic esophagitis, Schatzki ring, etc) were excluded from the main analyses. The primary outcome was failure to refer for HRM within one year of the index non-diagnostic EGD. We also investigated delayed referral for HRM, defined as HRM performed after the median. Multivariable logistic regression modeling was used to identify risk factors which independently predicted failure to refer for HRM, conditioned on the providing endoscopist.
Results: Among 2,132 patients who underwent EGD for dysphagia, 1,240 (58.2%) did not have findings to explain dysphagia on the index EGD. Of these 1,240 patients, 148 (11.9%) underwent HRM within one year of index EGD. Endoscopic findings that did not explain dysphagia (e.g., hiatal hernia, tortuous esophagus, Barrett’s esophagus, altered anatomy) were independently associated with failure to refer for HRM (aOR 0.45, 95% CI 0.25 – 0.80). Demographic factors including race/ethnicity, insurance type, and income were not associated with failure to refer for HRM or delayed HRM. Of HRMs performed, 42.6% showed a major motility disorder and 6.8% showed a minor motility disorder. The diagnosis of a major motility disorder found on HRM was similar among those who had incidental EGD findings that were non-diagnostic for dysphagia compared to those who had completely normal EGD findings (42.4% vs. 42.6%, p = 0.27).
Discussion: Findings unrelated to dysphagia appear to deter providers from referring for HRM despite its high yield.

Figure: A. Results of all patients HRM (n=148) for dysphagia subtyped into Normal, Major Motility Disorders, Minor Motility Disorders and Technically Limited HRM studies. B. Patients with Major Motility Disorders (n=63) classified by HRM results using the Chicago criteria.
Disclosures:
Sydney Pomenti indicated no relevant financial relationships.
John Nathanson indicated no relevant financial relationships.
Meaghan Phipps indicated no relevant financial relationships.
Chino Aneke-Nash indicated no relevant financial relationships.
David Katzka: Medtronic – Grant/Research Support.
Daniel Freedberg indicated no relevant financial relationships.
Daniela Jodorkovsky indicated no relevant financial relationships.
Sydney Pomenti, MD1, John Nathanson, MD2, Meaghan Phipps, MD1, Chino Aneke-Nash, MD, PhD1, David A.. Katzka, MD1, Daniel Freedberg, MD1, Daniela Jodorkovsky, MD3. P3252 - EGD Findings That Do No Not Explain Dysphagia Are Associated With Underutilization of High Resolution Manometry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
