Tuesday Poster Session
Category: Stomach
P4256 - Collagenous Gastritis: A Rare Cause of Dyspepsia in a Patient With Celiac Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- AS
Anjiya Shaikh, MBBS
University of Connecticut
Hartford, Connecticut
Presenting Author(s)
Anjiya Shaikh, MBBS1, Jaimy Villavicencio, MD1, Lisa Rossi, MD2
1University of Connecticut, Hartford, CT; 2Saint Francis Hospital-Trinity Health of New England, Hartford, CT
Introduction: Collagenous gastritis (CG) is a rare inflammatory disorder characterized by subepithelial collagen deposition and infiltration of mononuclear cells on gastric biopsy. Although the exact etiology of the disease remains unknown, the proposed pathogenesis includes chronic inflammation, drug-related reaction, and autoimmune injury. We report a rare case of collagenous gastritis presenting as dyspepsia in a patient with celiac disease.
Case Description/Methods: A 64-year-old female with history of celiac disease and hypothyroidism presented with a six-month history of worsening reflux disease. She also endorsed a month-long history of nausea and early satiety.
She reported her symptoms occurred despite strict adherence to a gluten-free diet (GFD). Furthermore, she denied any abdominal pain,dysphagia, or hematochezia.
Initial work-up was significant for a normal CBC, a positive ANA titer, a negative TTG IgA (demonstrating GFD compliance), and negative H. pylori testing. An upper GI series revealed an absence of the normal gastric mucosal pattern, with narrowing and stiffness of the gastric antrum.
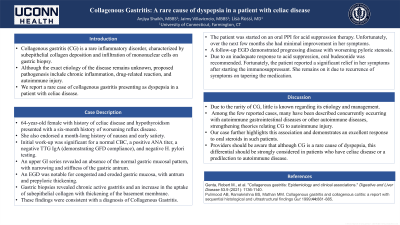
An EGD was notable for congested and eroded gastric mucosa, with antrum and prepyloric thickening. Gastric biopsies revealed chronic active gastritis and an increase in the uptake of subepithelial collagen with thickening of the basement membrane. These findings were consistent with a diagnosis of Collagenous Gastritis.
The patient was started on an oral PPI for acid suppression therapy. Unfortunately, over the next few months she had minimal improvement in her symptoms. A follow-up EGD demonstrated progressing disease with worsening pyloric stenosis. Due to an inadequate response to acid suppression, oral budesonide was recommended. Fortunately, the patient reported significant relief in her symptoms after starting the steroids. She remains on them as she had symptom recurrence on an attempted taper.
Discussion: Due to the rarity of CG, little is known regarding its etiology and management. Among the few reported cases, many concurrently occurred with autoimmune diseases such as lymphocytic gastritis, celiac disease, and others, strengthening theories relating CG to autoimmune injury. Our case not only further highlights this association but also demonstrates an excellent response to oral steroids in such patients. Providers should be aware that although CG is a rare cause of dyspepsia, this differential should be strongly considered in patients with celiac disease or a predilection to autoimmune disease.

Disclosures:
Anjiya Shaikh, MBBS1, Jaimy Villavicencio, MD1, Lisa Rossi, MD2. P4256 - Collagenous Gastritis: A Rare Cause of Dyspepsia in a Patient With Celiac Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Connecticut, Hartford, CT; 2Saint Francis Hospital-Trinity Health of New England, Hartford, CT
Introduction: Collagenous gastritis (CG) is a rare inflammatory disorder characterized by subepithelial collagen deposition and infiltration of mononuclear cells on gastric biopsy. Although the exact etiology of the disease remains unknown, the proposed pathogenesis includes chronic inflammation, drug-related reaction, and autoimmune injury. We report a rare case of collagenous gastritis presenting as dyspepsia in a patient with celiac disease.
Case Description/Methods: A 64-year-old female with history of celiac disease and hypothyroidism presented with a six-month history of worsening reflux disease. She also endorsed a month-long history of nausea and early satiety.
She reported her symptoms occurred despite strict adherence to a gluten-free diet (GFD). Furthermore, she denied any abdominal pain,dysphagia, or hematochezia.
Initial work-up was significant for a normal CBC, a positive ANA titer, a negative TTG IgA (demonstrating GFD compliance), and negative H. pylori testing. An upper GI series revealed an absence of the normal gastric mucosal pattern, with narrowing and stiffness of the gastric antrum.
An EGD was notable for congested and eroded gastric mucosa, with antrum and prepyloric thickening. Gastric biopsies revealed chronic active gastritis and an increase in the uptake of subepithelial collagen with thickening of the basement membrane. These findings were consistent with a diagnosis of Collagenous Gastritis.
The patient was started on an oral PPI for acid suppression therapy. Unfortunately, over the next few months she had minimal improvement in her symptoms. A follow-up EGD demonstrated progressing disease with worsening pyloric stenosis. Due to an inadequate response to acid suppression, oral budesonide was recommended. Fortunately, the patient reported significant relief in her symptoms after starting the steroids. She remains on them as she had symptom recurrence on an attempted taper.
Discussion: Due to the rarity of CG, little is known regarding its etiology and management. Among the few reported cases, many concurrently occurred with autoimmune diseases such as lymphocytic gastritis, celiac disease, and others, strengthening theories relating CG to autoimmune injury. Our case not only further highlights this association but also demonstrates an excellent response to oral steroids in such patients. Providers should be aware that although CG is a rare cause of dyspepsia, this differential should be strongly considered in patients with celiac disease or a predilection to autoimmune disease.

Figure: EGD demonstrates congested, eroded gastric mucosa with erythema and nodularity. Pre-pyloric thickening and stenosis were also noted.
Disclosures:
Anjiya Shaikh indicated no relevant financial relationships.
Jaimy Villavicencio indicated no relevant financial relationships.
Lisa Rossi indicated no relevant financial relationships.
Anjiya Shaikh, MBBS1, Jaimy Villavicencio, MD1, Lisa Rossi, MD2. P4256 - Collagenous Gastritis: A Rare Cause of Dyspepsia in a Patient With Celiac Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
