Tuesday Poster Session
Category: Esophagus
P3257 - Discrepancy in Esophageal Dysphagia Severity in Patients With Normal High-Resolution Manometry at a Safety Net vs Tertiary Hospital
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Chloe K. Tom, MD
Keck School of Medicine of USC
Los Angeles, CA
Presenting Author(s)
Chloe K. Tom, MD1, Ibrahim Abboud, BS2, Joshua Castle, BS1, Sonia Sharma, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1, Yan Jiang, MD1
1Keck School of Medicine of USC, Los Angeles, CA; 2Keck School of Medicine of USC and University of California, Riverside School of Medicine, Los Angeles, CA
Introduction: The association between dysphagia symptoms and high-resolution manometry (HRM) findings has not been well established in a safety-net hospital setting. Our group’s prior research found that patients with normal HRM findings at a safety-net hospital (site 1) had more severe dysphagia symptoms compared to those at an affiliated academic tertiary hospital (site 2). We aimed to evaluate the potential factors which may explain the disparity in reported dysphagia severity.
Methods: Adults undergoing HRM from January 2020 to March 2022 at sites 1 and 2 were prospectively administered brief esophageal dysphagia (BEDQ) and gastroesophageal reflux disease (GERDQ) questionnaires in validated English or Spanish versions according to preference. Demographics and esophagogastroduodenoscopy (EGD) findings from patients with normal HRM findings were collected. Multivariable linear regression was used to evaluate the impact of the hospital site on BEDQ scores after accounting for possible confounding factors.
Results: There was a total of 126 patients with normal HRM motility findings (39 site 1, 87 site 2). The mean BEDQ scores were 21.1 (site 1) and 9.7 (site 2) (p< 0.0001). Mean GERDQ scores were 8.9 (site 1) and 9.4 (site 2) (p=0.46). Sex and age were similar. At site 1, 37/39 (94.9%) patients were Hispanic vs. 22/86 (25.6%) at site 2. EGD findings were mainly normal at both sites. Esophagitis was more prevalent at site 2 (16.9% vs 8.1%). Hiatal hernia was more common at site 2 (47.1% vs 33.3%). At site 2, most HRM was performed for indication of GERD (N=38, 43.7%), dysphagia (N=30, 34.5%) and hiatal hernia (N=9, 10.3%). At site 1, the most common indications were dysphagia (N=25, 64.1%) and GERD (N=11, 28.2%). BEDQ scores varied based on manometry indication but were consistently higher at site 1. After adjusting for factors (age, sex, ethnicity, BMI, presence of hiatal hernia, HRM indication, and EGD findings), hospital site was still a significant variable affecting BEDQ scores (p=0.045).
Discussion: In patients with normal HRM findings, esophageal dysphagia symptoms were more severe at a safety net hospital compared to an affiliated tertiary academic hospital, even after controlling for variables such as HRM indication, EGD findings, and ethnicity. This interesting finding suggests other factors may contribute to symptom disparity. Investigation is warranted to evaluate if there are explanatory socioeconomic variables and assess validity of dysphagia surveys in the underserved patient population.

Disclosures:
Chloe K. Tom, MD1, Ibrahim Abboud, BS2, Joshua Castle, BS1, Sonia Sharma, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1, Yan Jiang, MD1. P3257 - Discrepancy in Esophageal Dysphagia Severity in Patients With Normal High-Resolution Manometry at a Safety Net vs Tertiary Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Keck School of Medicine of USC, Los Angeles, CA; 2Keck School of Medicine of USC and University of California, Riverside School of Medicine, Los Angeles, CA
Introduction: The association between dysphagia symptoms and high-resolution manometry (HRM) findings has not been well established in a safety-net hospital setting. Our group’s prior research found that patients with normal HRM findings at a safety-net hospital (site 1) had more severe dysphagia symptoms compared to those at an affiliated academic tertiary hospital (site 2). We aimed to evaluate the potential factors which may explain the disparity in reported dysphagia severity.
Methods: Adults undergoing HRM from January 2020 to March 2022 at sites 1 and 2 were prospectively administered brief esophageal dysphagia (BEDQ) and gastroesophageal reflux disease (GERDQ) questionnaires in validated English or Spanish versions according to preference. Demographics and esophagogastroduodenoscopy (EGD) findings from patients with normal HRM findings were collected. Multivariable linear regression was used to evaluate the impact of the hospital site on BEDQ scores after accounting for possible confounding factors.
Results: There was a total of 126 patients with normal HRM motility findings (39 site 1, 87 site 2). The mean BEDQ scores were 21.1 (site 1) and 9.7 (site 2) (p< 0.0001). Mean GERDQ scores were 8.9 (site 1) and 9.4 (site 2) (p=0.46). Sex and age were similar. At site 1, 37/39 (94.9%) patients were Hispanic vs. 22/86 (25.6%) at site 2. EGD findings were mainly normal at both sites. Esophagitis was more prevalent at site 2 (16.9% vs 8.1%). Hiatal hernia was more common at site 2 (47.1% vs 33.3%). At site 2, most HRM was performed for indication of GERD (N=38, 43.7%), dysphagia (N=30, 34.5%) and hiatal hernia (N=9, 10.3%). At site 1, the most common indications were dysphagia (N=25, 64.1%) and GERD (N=11, 28.2%). BEDQ scores varied based on manometry indication but were consistently higher at site 1. After adjusting for factors (age, sex, ethnicity, BMI, presence of hiatal hernia, HRM indication, and EGD findings), hospital site was still a significant variable affecting BEDQ scores (p=0.045).
Discussion: In patients with normal HRM findings, esophageal dysphagia symptoms were more severe at a safety net hospital compared to an affiliated tertiary academic hospital, even after controlling for variables such as HRM indication, EGD findings, and ethnicity. This interesting finding suggests other factors may contribute to symptom disparity. Investigation is warranted to evaluate if there are explanatory socioeconomic variables and assess validity of dysphagia surveys in the underserved patient population.

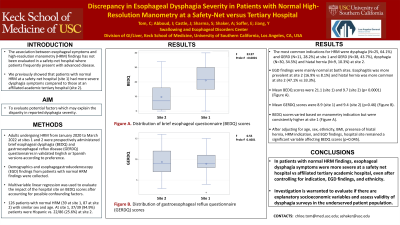
Figure: Figure 1
A. Distribution of brief esophageal dysphagia questionnaire (BEDQ) scores
B. Distribution of gastroesophageal reflux disease questionnaire (GERDQ) scores
A. Distribution of brief esophageal dysphagia questionnaire (BEDQ) scores
B. Distribution of gastroesophageal reflux disease questionnaire (GERDQ) scores
Disclosures:
Chloe Tom indicated no relevant financial relationships.
Ibrahim Abboud indicated no relevant financial relationships.
Joshua Castle indicated no relevant financial relationships.
Sonia Sharma indicated no relevant financial relationships.
Anisa Shaker indicated no relevant financial relationships.
Edy Soffer indicated no relevant financial relationships.
Yan Jiang indicated no relevant financial relationships.
Chloe K. Tom, MD1, Ibrahim Abboud, BS2, Joshua Castle, BS1, Sonia Sharma, MD1, Anisa Shaker, MD1, Edy Soffer, MD, FACG1, Yan Jiang, MD1. P3257 - Discrepancy in Esophageal Dysphagia Severity in Patients With Normal High-Resolution Manometry at a Safety Net vs Tertiary Hospital, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
