Tuesday Poster Session
Category: Esophagus
P3260 - Primary Care Provider Perspectives on Facilitators and Barriers to Barrett’s Screening: Results from a Qualitative Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Swathi Eluri, MD, MSCR
University of North Carolina School of Medicine
Chapel Hill, North Carolina
Presenting Author(s)
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Universty of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Despite screening guidelines for Barrett’s esophagus (BE), only a small proportion of esophageal adenocarcinoma (EAC) patients have known prior BE. Since most patients are seen in primary care, optimizing screening at the primary care level is critical. The aim is to identify primary care provider-specific barriers and facilitators to BE screening using in-depth qualitative interviews.
Methods: In this qualitative study, family medicine (FM) or internal medicine (IM) providers were recruited to participate in in-depth interviews lasting 45-60 minutes and conducted by trained qualitative research specialists. Interviewers followed an exploratory and interactive interview guide. All interviews were digitally recorded, transcribed, and analyzed using qualitative research software. Saturation of themes was reached after 10 interviews. The initial codebook was pilot tested and refined. Standard consensus coding guidelines were followed. Code reports for each code and narrative summaries, themes, sub-themes, and illustrative quotes, were generated.
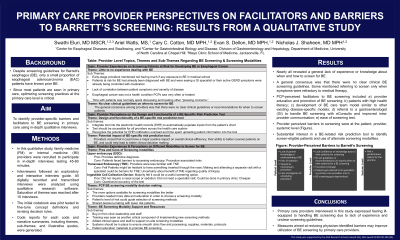
Results: Of the 10 providers, 60% were female and 90% were IM vs 10% FM. Themes and sub-themes were divided into three main topics areas (Table). Nearly all revealed a general lack of experience or knowledge about when and how to screen for BE, regardless of years in practice. A general consensus was that there were no clear clinical BE screening guidelines or recommendations. Some mentioned referring to screen only with refractory symptoms. PCP-perceived facilitators to BE screening included a) provider education and promotion of BE screening; b) patients with high health literacy; c) development of BE care team model similar to other existing disease-specific models; d) referral to a gastroenterologist (GI) to handle BE screening with eConsults and improved intra-provider communication; e) ease of screening test. Provider perceived screening barriers were at the patient, provider, systemic level (Figure). Providers revealed substantial interest in a BE-related risk prediction tool to identify screen-eligible patients. Providers were also receptive to use of alternate screening modalities (Table) if there was adequate support and infrastructure.
Discussion: Primary care providers interviewed in this study expressed feeling ill-equipped to handling BE screening due to lack of experience and unclear screening guidelines. Measures aimed at reducing physician-identified barriers may improve utilization of BE screening by primary care providers.

Disclosures:
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2. P3260 - Primary Care Provider Perspectives on Facilitators and Barriers to Barrett’s Screening: Results from a Qualitative Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Universty of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Despite screening guidelines for Barrett’s esophagus (BE), only a small proportion of esophageal adenocarcinoma (EAC) patients have known prior BE. Since most patients are seen in primary care, optimizing screening at the primary care level is critical. The aim is to identify primary care provider-specific barriers and facilitators to BE screening using in-depth qualitative interviews.
Methods: In this qualitative study, family medicine (FM) or internal medicine (IM) providers were recruited to participate in in-depth interviews lasting 45-60 minutes and conducted by trained qualitative research specialists. Interviewers followed an exploratory and interactive interview guide. All interviews were digitally recorded, transcribed, and analyzed using qualitative research software. Saturation of themes was reached after 10 interviews. The initial codebook was pilot tested and refined. Standard consensus coding guidelines were followed. Code reports for each code and narrative summaries, themes, sub-themes, and illustrative quotes, were generated.
Results: Of the 10 providers, 60% were female and 90% were IM vs 10% FM. Themes and sub-themes were divided into three main topics areas (Table). Nearly all revealed a general lack of experience or knowledge about when and how to screen for BE, regardless of years in practice. A general consensus was that there were no clear clinical BE screening guidelines or recommendations. Some mentioned referring to screen only with refractory symptoms. PCP-perceived facilitators to BE screening included a) provider education and promotion of BE screening; b) patients with high health literacy; c) development of BE care team model similar to other existing disease-specific models; d) referral to a gastroenterologist (GI) to handle BE screening with eConsults and improved intra-provider communication; e) ease of screening test. Provider perceived screening barriers were at the patient, provider, systemic level (Figure). Providers revealed substantial interest in a BE-related risk prediction tool to identify screen-eligible patients. Providers were also receptive to use of alternate screening modalities (Table) if there was adequate support and infrastructure.
Discussion: Primary care providers interviewed in this study expressed feeling ill-equipped to handling BE screening due to lack of experience and unclear screening guidelines. Measures aimed at reducing physician-identified barriers may improve utilization of BE screening by primary care providers.

Figure: Primary Care Provider Perceived Barriers to Barrett’s Screening
Disclosures:
Swathi Eluri indicated no relevant financial relationships.
Ariel Watts indicated no relevant financial relationships.
Cary Cotton indicated no relevant financial relationships.
Evan Dellon indicated no relevant financial relationships.
Nicholas Shaheen indicated no relevant financial relationships.
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2. P3260 - Primary Care Provider Perspectives on Facilitators and Barriers to Barrett’s Screening: Results from a Qualitative Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
