Tuesday Poster Session
Category: Esophagus
P3261 - Using In-Depth Patient Interviews to Understand Patient Perspectives and Experience on Barrett’s Esophagus Screening
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Swathi Eluri, MD, MSCR
University of North Carolina School of Medicine
Chapel Hill, North Carolina
Presenting Author(s)
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Universty of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Two-thirds of screen-eligible patients for Barrett’s esophagus (BE) never undergo an upper endoscopy (EGD). Little is known about patient-specific factors affecting BE screening. The aim is to identify patient perspectives on gastroesophageal reflux disease (GERD), BE, and barriers and facilitators to BE screening.
Methods: This is a qualitative study using in-depth interviews of 45-60 minutes. Subjects were screen-eligible adults per ACG BE guidelines: chronic/symptomatic GERD & ³2 risk factors. 21 interviews were conducted by trained qualitative specialists until thematic saturation. An exploratory and interactive interview guide was developed to elicit patient insight and descriptive detail. Interviews were digitally recorded, transcribed, and analyzed using qualitative research software. The initial codebook was pilot tested and refined. Standard consensus coding guidelines were followed. Code reports for each code and narrative summaries were generated.
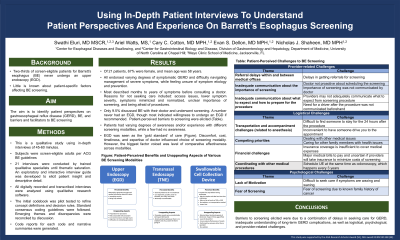
Results: Of 21 patients, 67% were female, and mean age was 58 years. All endorsed varying degrees of symptomatic GERD and difficulty navigating management of painful, sometimes severe symptoms, while feeling unsure of symptom etiology and prevention. Most described months to years of symptoms before consulting a doctor. Reasons for not seeking care included: access issues, lower symptom severity, symptoms minimized and normalized, unclear importance of screening, and being afraid of procedures. Responses varied about long-term implications of GERD and awareness of BE. Some were aware of BE, but did not receive information from a doctor. Only 9.5% discussed BE with their doctor and underwent screening. A number never had an EGD, though most indicated willingness to undergo an EGD if recommended. Patient-perceived barriers to screening were elicited (Table). Patients had varying degrees of awareness and/or experience with different screening modalities, while a few had no awareness. EGD was seen as the ‘gold standard’ of care (Figure). There were mixed responses to sedation. Discomfort, cost, timeliness, and expertise of doctor influenced choice of screening modality. However, the biggest factor voiced was level of comparative effectiveness across modalities.
Discussion: Barriers to screening elicited were due to a combination of delays in seeking care for GERD, inadequate understanding of long-term GERD complications, as well as logistical, psychological, and provider-related challenges.

Disclosures:
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2. P3261 - Using In-Depth Patient Interviews to Understand Patient Perspectives and Experience on Barrett’s Esophagus Screening, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Universty of North Carolina School of Medicine, Chapel Hill, NC
Introduction: Two-thirds of screen-eligible patients for Barrett’s esophagus (BE) never undergo an upper endoscopy (EGD). Little is known about patient-specific factors affecting BE screening. The aim is to identify patient perspectives on gastroesophageal reflux disease (GERD), BE, and barriers and facilitators to BE screening.
Methods: This is a qualitative study using in-depth interviews of 45-60 minutes. Subjects were screen-eligible adults per ACG BE guidelines: chronic/symptomatic GERD & ³2 risk factors. 21 interviews were conducted by trained qualitative specialists until thematic saturation. An exploratory and interactive interview guide was developed to elicit patient insight and descriptive detail. Interviews were digitally recorded, transcribed, and analyzed using qualitative research software. The initial codebook was pilot tested and refined. Standard consensus coding guidelines were followed. Code reports for each code and narrative summaries were generated.
Results: Of 21 patients, 67% were female, and mean age was 58 years. All endorsed varying degrees of symptomatic GERD and difficulty navigating management of painful, sometimes severe symptoms, while feeling unsure of symptom etiology and prevention. Most described months to years of symptoms before consulting a doctor. Reasons for not seeking care included: access issues, lower symptom severity, symptoms minimized and normalized, unclear importance of screening, and being afraid of procedures. Responses varied about long-term implications of GERD and awareness of BE. Some were aware of BE, but did not receive information from a doctor. Only 9.5% discussed BE with their doctor and underwent screening. A number never had an EGD, though most indicated willingness to undergo an EGD if recommended. Patient-perceived barriers to screening were elicited (Table). Patients had varying degrees of awareness and/or experience with different screening modalities, while a few had no awareness. EGD was seen as the ‘gold standard’ of care (Figure). There were mixed responses to sedation. Discomfort, cost, timeliness, and expertise of doctor influenced choice of screening modality. However, the biggest factor voiced was level of comparative effectiveness across modalities.
Discussion: Barriers to screening elicited were due to a combination of delays in seeking care for GERD, inadequate understanding of long-term GERD complications, as well as logistical, psychological, and provider-related challenges.

Figure: Patient-Perceived Benefits and Unappealing Aspects of Various BE Screening Modalities
Disclosures:
Swathi Eluri indicated no relevant financial relationships.
Ariel Watts indicated no relevant financial relationships.
Cary Cotton indicated no relevant financial relationships.
Evan Dellon indicated no relevant financial relationships.
Nicholas Shaheen indicated no relevant financial relationships.
Swathi Eluri, MD, MSCR1, Ariel Watts, MS1, Cary C.. Cotton, MD, MPH1, Evan S. Dellon, MD, MPH1, Nicholas Shaheen, MD, MPH2. P3261 - Using In-Depth Patient Interviews to Understand Patient Perspectives and Experience on Barrett’s Esophagus Screening, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
