Tuesday Poster Session
Category: Esophagus
P3263 - Esophageal Dysmotility Patterns in Veterans With Diabetes: A Retrospective Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Abu Abbasi, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Abu Fahad Abbasi, MD1, Jeffrey Leya, MD2, Josh Kalapala, 1, Promila Banerjee, MD3, Stephen Sonntag, MD4
1Loyola University Medical Center, Maywood, IL; 2Loyola University Medical Center, Barrington, IL; 3Loyola University Medical Center, Hines, IL; 4Loyola University Medical Center, Hines, IL
Introduction: Diabetes mellitus (DM) can lead to gastrointestinal complications, including esophageal dysmotility that contribute to GERD and affect patients' quality of life. This study aims to examine the relationship between diabetes mellitus and esophageal dysmotilities in a veteran patient population, investigating various dysmotility diagnoses.
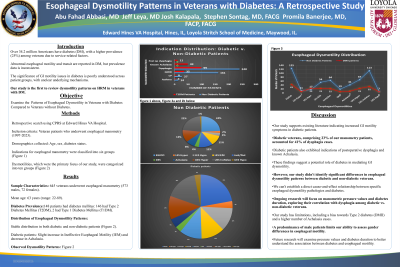
Methods: A retrospective database search was conducted using the Computerized Patient Record System (CPRS) at Edward Hines VA Hospital. Our patient sample population included veteran patients who underwent esophageal manometry between 1997 and 2022. The patient demographics including age, sex, and presence or absence of diabetes were collected. Patients were further divided into diagnoses of Type 1 Diabetes Mellitus (T1DM) and Type 2 Diabetes Mellitus (T2DM. Results of the esophageal manometries for all patients were analyzed and separated into 9 diagnoses. (Figure 1-2)
Results: Among the 619 patients who underwent esophageal manometry, median age of the patients was 68 years, with a wide age range (22-89 years). Of these patients, 148 patients had diabetes mellitus. Specifically, 146 had T2DM and 2 had T1DM. There was a relatively stable distribution of esophageal dysmotility patterns among diabetic and non-diabetic patients. (Figures 1-2). Notably, there was a slight increase in proportion of those with Ineffective Esophageal Motility (IEM) as well as a slight decrease in proportion of Achalasia diagnoses among the diabetic patients. Various patterns of esophageal dysmotility were observed, including UES hypertension/hypotension, achalasia, EGJ outflow obstruction, distal esophageal spasm, ineffective esophageal motility, hypercontractile esophagus, LES hypotension, and normal motility.
Discussion: This study shows significant presence of esophageal dysmotility in veterans with diabetes, particularly T2DM. The findings underscore the importance of recognizing and evaluating esophageal dysmotility in individuals with diabetes to provide appropriate management and improve patient outcomes. We are the first study to separate esophageal dysmotility patterns based on diabetic diagnosis. These findings are preliminary and further analysis will be continued to more precisely assess whether the presence of diabetes will lead to specific types of dysmotilities over others. Additionally we plan to assess how duration of diabetes leads to esophageal dysmotilities.

Disclosures:
Abu Fahad Abbasi, MD1, Jeffrey Leya, MD2, Josh Kalapala, 1, Promila Banerjee, MD3, Stephen Sonntag, MD4. P3263 - Esophageal Dysmotility Patterns in Veterans With Diabetes: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Loyola University Medical Center, Barrington, IL; 3Loyola University Medical Center, Hines, IL; 4Loyola University Medical Center, Hines, IL
Introduction: Diabetes mellitus (DM) can lead to gastrointestinal complications, including esophageal dysmotility that contribute to GERD and affect patients' quality of life. This study aims to examine the relationship between diabetes mellitus and esophageal dysmotilities in a veteran patient population, investigating various dysmotility diagnoses.
Methods: A retrospective database search was conducted using the Computerized Patient Record System (CPRS) at Edward Hines VA Hospital. Our patient sample population included veteran patients who underwent esophageal manometry between 1997 and 2022. The patient demographics including age, sex, and presence or absence of diabetes were collected. Patients were further divided into diagnoses of Type 1 Diabetes Mellitus (T1DM) and Type 2 Diabetes Mellitus (T2DM. Results of the esophageal manometries for all patients were analyzed and separated into 9 diagnoses. (Figure 1-2)
Results: Among the 619 patients who underwent esophageal manometry, median age of the patients was 68 years, with a wide age range (22-89 years). Of these patients, 148 patients had diabetes mellitus. Specifically, 146 had T2DM and 2 had T1DM. There was a relatively stable distribution of esophageal dysmotility patterns among diabetic and non-diabetic patients. (Figures 1-2). Notably, there was a slight increase in proportion of those with Ineffective Esophageal Motility (IEM) as well as a slight decrease in proportion of Achalasia diagnoses among the diabetic patients. Various patterns of esophageal dysmotility were observed, including UES hypertension/hypotension, achalasia, EGJ outflow obstruction, distal esophageal spasm, ineffective esophageal motility, hypercontractile esophagus, LES hypotension, and normal motility.
Discussion: This study shows significant presence of esophageal dysmotility in veterans with diabetes, particularly T2DM. The findings underscore the importance of recognizing and evaluating esophageal dysmotility in individuals with diabetes to provide appropriate management and improve patient outcomes. We are the first study to separate esophageal dysmotility patterns based on diabetic diagnosis. These findings are preliminary and further analysis will be continued to more precisely assess whether the presence of diabetes will lead to specific types of dysmotilities over others. Additionally we plan to assess how duration of diabetes leads to esophageal dysmotilities.

Figure: Figure 1: A Comparison of Esophageal Dysmotility Distribution Among Diabetic and Non-Diabetic Patients
Disclosures:
Abu Fahad Abbasi indicated no relevant financial relationships.
Jeffrey Leya indicated no relevant financial relationships.
Josh Kalapala indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Stephen Sonntag indicated no relevant financial relationships.
Abu Fahad Abbasi, MD1, Jeffrey Leya, MD2, Josh Kalapala, 1, Promila Banerjee, MD3, Stephen Sonntag, MD4. P3263 - Esophageal Dysmotility Patterns in Veterans With Diabetes: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
