Tuesday Poster Session
Category: Esophagus
P3264 - The Tissue Systems Pathology Test Predicts Risk of Progression in Medicare-Eligible Patients with Barrett’s Esophagus
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Harshit S. Khara, MD
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Award: Presidential Poster Award
Harshit S. Khara, MD1, Jon M.. Davison, MD2, John Goldblum, MD3, Prashanthi N. Thota, MD4, Lucas C.. Duits, MD, PhD5, Amir Khoshiwal, MSc5, Jacques J.. Bergman, MD, PhD5, Gary Falk, MD, MS, FACG6, Christian Smolko, PhD7, Mary Hall, MBA, PhD7, Jennifer J. Siegel, MA, PhD8, Rebecca J. Critchley-Thorne, PhD7, David L. Diehl, MD1
1Geisinger Medical Center, Danville, PA; 2University of Pittsburgh School of Medicine, Pittsburgh, PA; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5Amsterdam University Medical Center, Amsterdam, Noord-Holland, Netherlands; 6University of Pennsylvania Perelman School of Medicine, Philadelphia, PA; 7Castle Biosciences, Pittsburgh, PA; 8Castle Biosciences, Friendswood, TX
Introduction: Accurate prediction of risk of progression to esophageal adenocarcinoma (EAC) is needed in patients with Barrett’s esophagus (BE), which disproportionately affects patients ≥ 65 years of age (Medicare-eligible), representing the majority of EAC cases diagnosed each year in the U.S. Multiple studies have validated that the tissue systems pathology (TSP-9) test predicts risk of neoplastic progression in patients with BE. This study evaluated the performance of TSP-9 for predicting risk of progression to high-grade dysplasia (HGD) or EAC in Medicare-eligible BE patients.
Methods: A pooled analysis was performed on data from 5 studies of 290 BE patients who were ≥ 65 years old with known outcomes, including 84 patients who progressed to HGD/EAC in 2.4 years (median; IQR 1.3 - 3.5). Data were also analyzed from a second cohort on clinical use of the TSP-9 test ordered by 356 physicians at 251 clinical sites for 2,078 BE patients ≥ 65 years old. The risk stratification performance of TSP-9 results and clinicopathologic variables was evaluated.
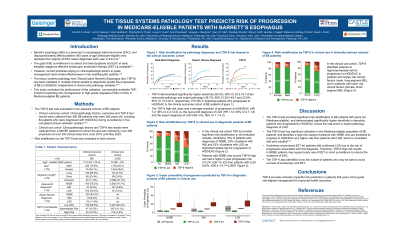
Results: In the pooled analysis of patients with known outcomes, TSP-9 demonstrated significantly higher sensitivity (64.0%; 95% CI 53.3 - 74.7) than expert pathology and real-world pathology (22.6%; 95% CI 13.3 - 33.3 and 38.7%; 95% CI 28.0 - 49.3, respectively; P < 0.05) in detecting patients who progressed to HGD/EAC. In multivariable analyses with clinicopathologic variables, TSP-9 was the strongest, independent predictor of progression to HGD/EAC (HR 7.2; 95% CI 4.2 - 14.2; P < 0.0001; Table, Fig. 1A). In the clinical use cohort, TSP-9 provided significant risk stratification in all evaluated subsets, identifying 17.7% of patients as high/intermediate risk for progression to HGD/EAC (Fig. 1B-E). Patients with NDBE who scored TSP-9 high risk had a higher 5-year progression risk (16.6%; IQR 13.7 - 25.0) than patients with LGD (6.1%; IQR 3.0 - 14.5; Fig. 1B).
Discussion: The TSP-9 test risk-stratifies BE patients ≥ 65 years old independently of clinicopathologic variables and has significantly higher sensitivity for detection of progressors than pathology diagnosis of LGD. In clinical use, the TSP-9 test identified a high-risk subset of NDBE patients who had a higher progression risk than patients with LGD, enabling early detection of patients requiring escalation of care to reduce the incidence of EAC. TSP-9 provides clinically impactful risk prediction in patients ≥ 65 years old to guide risk-aligned care for improved health outcomes.

Disclosures:
Harshit S. Khara, MD1, Jon M.. Davison, MD2, John Goldblum, MD3, Prashanthi N. Thota, MD4, Lucas C.. Duits, MD, PhD5, Amir Khoshiwal, MSc5, Jacques J.. Bergman, MD, PhD5, Gary Falk, MD, MS, FACG6, Christian Smolko, PhD7, Mary Hall, MBA, PhD7, Jennifer J. Siegel, MA, PhD8, Rebecca J. Critchley-Thorne, PhD7, David L. Diehl, MD1. P3264 - The Tissue Systems Pathology Test Predicts Risk of Progression in Medicare-Eligible Patients with Barrett’s Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Harshit S. Khara, MD1, Jon M.. Davison, MD2, John Goldblum, MD3, Prashanthi N. Thota, MD4, Lucas C.. Duits, MD, PhD5, Amir Khoshiwal, MSc5, Jacques J.. Bergman, MD, PhD5, Gary Falk, MD, MS, FACG6, Christian Smolko, PhD7, Mary Hall, MBA, PhD7, Jennifer J. Siegel, MA, PhD8, Rebecca J. Critchley-Thorne, PhD7, David L. Diehl, MD1
1Geisinger Medical Center, Danville, PA; 2University of Pittsburgh School of Medicine, Pittsburgh, PA; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5Amsterdam University Medical Center, Amsterdam, Noord-Holland, Netherlands; 6University of Pennsylvania Perelman School of Medicine, Philadelphia, PA; 7Castle Biosciences, Pittsburgh, PA; 8Castle Biosciences, Friendswood, TX
Introduction: Accurate prediction of risk of progression to esophageal adenocarcinoma (EAC) is needed in patients with Barrett’s esophagus (BE), which disproportionately affects patients ≥ 65 years of age (Medicare-eligible), representing the majority of EAC cases diagnosed each year in the U.S. Multiple studies have validated that the tissue systems pathology (TSP-9) test predicts risk of neoplastic progression in patients with BE. This study evaluated the performance of TSP-9 for predicting risk of progression to high-grade dysplasia (HGD) or EAC in Medicare-eligible BE patients.
Methods: A pooled analysis was performed on data from 5 studies of 290 BE patients who were ≥ 65 years old with known outcomes, including 84 patients who progressed to HGD/EAC in 2.4 years (median; IQR 1.3 - 3.5). Data were also analyzed from a second cohort on clinical use of the TSP-9 test ordered by 356 physicians at 251 clinical sites for 2,078 BE patients ≥ 65 years old. The risk stratification performance of TSP-9 results and clinicopathologic variables was evaluated.
Results: In the pooled analysis of patients with known outcomes, TSP-9 demonstrated significantly higher sensitivity (64.0%; 95% CI 53.3 - 74.7) than expert pathology and real-world pathology (22.6%; 95% CI 13.3 - 33.3 and 38.7%; 95% CI 28.0 - 49.3, respectively; P < 0.05) in detecting patients who progressed to HGD/EAC. In multivariable analyses with clinicopathologic variables, TSP-9 was the strongest, independent predictor of progression to HGD/EAC (HR 7.2; 95% CI 4.2 - 14.2; P < 0.0001; Table, Fig. 1A). In the clinical use cohort, TSP-9 provided significant risk stratification in all evaluated subsets, identifying 17.7% of patients as high/intermediate risk for progression to HGD/EAC (Fig. 1B-E). Patients with NDBE who scored TSP-9 high risk had a higher 5-year progression risk (16.6%; IQR 13.7 - 25.0) than patients with LGD (6.1%; IQR 3.0 - 14.5; Fig. 1B).
Discussion: The TSP-9 test risk-stratifies BE patients ≥ 65 years old independently of clinicopathologic variables and has significantly higher sensitivity for detection of progressors than pathology diagnosis of LGD. In clinical use, the TSP-9 test identified a high-risk subset of NDBE patients who had a higher progression risk than patients with LGD, enabling early detection of patients requiring escalation of care to reduce the incidence of EAC. TSP-9 provides clinically impactful risk prediction in patients ≥ 65 years old to guide risk-aligned care for improved health outcomes.

Figure: Figure 1. TSP-9 provides significant risk stratification in BE patients ≥65 years old. A: Kaplan-Meier analysis of TSP-9 risk classes for 290 patients with BE (NDBE, n=160; IND, n=27; and LGD, n=103), including 84 patients who progressed to HGD/EAC within 2.4 years (median; IQR, 1.3–3.5) and 206 patients with a median follow-up of 6.1 years (IQR, 4.7–7.7) with no disease progression. B: The 5-year probability of progression to HGD/EAC predicted by TSP-9 in clinical use in 2,078 patients with NDBE (n=1,862), IND (n=104), or LGD (n=77). C: Risk stratification by TSP-9 in clinical use for patients with NDBE (n=1,862), IND (n=104), or LGD (n=77); female (n=765) and male (n=1,313) BE patients; and patients with short- (n=67) or long-segment (n=64) BE. TSP-9, Tissue Systems Pathology-9 test; BE, Barrett's esophagus; Int, intermediate; NDBE, non-dysplastic Barrett’s esophagus; IND, indefinite for dysplasia; LGD, low-grade dysplasia.
Disclosures:
Harshit Khara: Boston Scientific – Consultant, Speakers Bureau. Castle Biosciences – Consultant, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook Medical – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus America – Consultant, Speakers Bureau. Pentax – Consultant, Speakers Bureau.
Jon Davison: Castle Biosciences, Inc. and Cernostics, Inc. (a wholly owned subsidiary of Castle Biosciences, Inc.) – Consultant.
John Goldblum indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Lucas Duits indicated no relevant financial relationships.
Amir Khoshiwal indicated no relevant financial relationships.
Jacques Bergman: Cernostics, Inc. (a wholly owned subsidiary of Castle Biosciences, Inc.), CDx Diagnostics, and Lucid Diagnostics – Grant/Research Support.
Gary Falk: Castle Bioscience – Grant/Research Support. EXACT – Consultant. Phathom – Consultant.
Christian Smolko: Castle Biosciences – Employee, Stock-publicly held company(excluding mutual/index funds).
Mary Hall: Castle Biosciences, Inc. – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Jennifer Siegel: Castle Biosciences Inc – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Rebecca J. Critchley-Thorne: Castle Biosciences – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
David Diehl: Boston Scientific – Consultant. Castle – Consultant. Laborie – Consultant. Merit Endotek – Consultant. Microtech – Consultant. Olympus – Consultant. OnePass Medical – Consultant. Pentax – Consultant. Steris – Consultant.
Harshit S. Khara, MD1, Jon M.. Davison, MD2, John Goldblum, MD3, Prashanthi N. Thota, MD4, Lucas C.. Duits, MD, PhD5, Amir Khoshiwal, MSc5, Jacques J.. Bergman, MD, PhD5, Gary Falk, MD, MS, FACG6, Christian Smolko, PhD7, Mary Hall, MBA, PhD7, Jennifer J. Siegel, MA, PhD8, Rebecca J. Critchley-Thorne, PhD7, David L. Diehl, MD1. P3264 - The Tissue Systems Pathology Test Predicts Risk of Progression in Medicare-Eligible Patients with Barrett’s Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

