Tuesday Poster Session
Category: Esophagus
P3265 - The Tissue Systems Pathology Test Objectively Risk-Stratifies Patients with Barrett’s Esophagus: A Multicenter US Clinical Experience Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Harshit S. Khara, MD
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Harshit S. Khara, MD1, Michael Yodice, MD1, Nicolas Villa, MD2, Miguel Ordonez-Castellanos, MD3, Christian Smolko, PhD4, Meenakshi Arora, PhD4, Rebecca J. Critchley-Thorne, PhD4, David L. Diehl, MD1
1Geisinger Medical Center, Danville, PA; 2MultiCare Rockwood Digestive Health Center, Spokane, WA; 3MultiCare Rockwood Digestive Health Center, Spokane, WI; 4Castle Biosciences, Pittsburgh, PA
Introduction: Endoscopic surveillance of Barrett’s esophagus (BE) is recommended to detect and treat malignant progression at early stages. However, current clinical practices have limited effectiveness in risk-stratifying BE patients. This study evaluated the performance of the validated, commercially available tissue systems pathology test (TissueCypher, TSP-9) to risk-stratify clinically relevant subsets of BE patients.
Methods: Data from clinical use of the TSP-9 test ordered by 475 physicians at 325 clinical sites for 3,935 patients were analyzed. Orders were from community (92.8%) and academic (7.2%) settings for patients with pathology diagnoses of non-dysplastic BE (NDBE, n=3,553), indefinite for dysplasia (IND, n=190, 4.8%), low-grade dysplasia (LGD, n=112, 2.8%) or BE with no graded assessment (n=80, 2.0%). TSP-9 risk results and predicted probability of progression to high-grade dysplasia (HGD)/esophageal adenocarcinoma (EAC) within 5 years were evaluated within clinically relevant patient subsets.
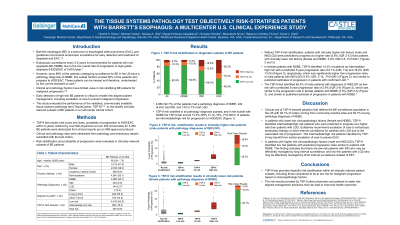
Results: The TSP-9 test provided significant risk stratification independent of clinicopathologic factors (Fig. 1). Patients with clinically higher risk factors (male and IND/LGD) were predicted to progress at a higher rate (4.8%; IQR 2-12) than patients with clinically lower risk factors (female and NDBE, 3.0%; IQR 1.8-5.1, P< 0.0001, Table 1). In NDBE female patients, TSP-9 identified 15.2% of patients as intermediate/high risk for progression with a predicted 5-year progression rate of 8.1% (IQR, 7-9) and 16.6% (IQR, 13-26), respectively, which was significantly higher than progression rates in males with IND/LGD (4.8%; IQR, 2-12) (P< 0.0001, Fig. 1B-C). The TSP-9 test identified 71.4% of IND/LGD male patients as low-risk with a predicted 5-year progression rate of 2.8% (IQR 2-4), which can enable confidence in a surveillance-only approach (Fig. 1C).
Discussion: The TSP-9 test provided significant risk stratification in clinical practice, including in patients considered to be at low risk for malignant progression based on clinicopathologic features. TSP-9 identified 15.2% of NDBE females as intermediate/high-risk for progression providing objective results to guide escalation of care with the goal of preventing EAC. The test also identified low-risk patients who can safely be managed by surveillance. Clinically impactful risk stratification by TSP-9 can allow physicians to consider risk-aligned management options with their patients to improve health outcomes.

Disclosures:
Harshit S. Khara, MD1, Michael Yodice, MD1, Nicolas Villa, MD2, Miguel Ordonez-Castellanos, MD3, Christian Smolko, PhD4, Meenakshi Arora, PhD4, Rebecca J. Critchley-Thorne, PhD4, David L. Diehl, MD1. P3265 - The Tissue Systems Pathology Test Objectively Risk-Stratifies Patients with Barrett’s Esophagus: A Multicenter US Clinical Experience Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2MultiCare Rockwood Digestive Health Center, Spokane, WA; 3MultiCare Rockwood Digestive Health Center, Spokane, WI; 4Castle Biosciences, Pittsburgh, PA
Introduction: Endoscopic surveillance of Barrett’s esophagus (BE) is recommended to detect and treat malignant progression at early stages. However, current clinical practices have limited effectiveness in risk-stratifying BE patients. This study evaluated the performance of the validated, commercially available tissue systems pathology test (TissueCypher, TSP-9) to risk-stratify clinically relevant subsets of BE patients.
Methods: Data from clinical use of the TSP-9 test ordered by 475 physicians at 325 clinical sites for 3,935 patients were analyzed. Orders were from community (92.8%) and academic (7.2%) settings for patients with pathology diagnoses of non-dysplastic BE (NDBE, n=3,553), indefinite for dysplasia (IND, n=190, 4.8%), low-grade dysplasia (LGD, n=112, 2.8%) or BE with no graded assessment (n=80, 2.0%). TSP-9 risk results and predicted probability of progression to high-grade dysplasia (HGD)/esophageal adenocarcinoma (EAC) within 5 years were evaluated within clinically relevant patient subsets.
Results: The TSP-9 test provided significant risk stratification independent of clinicopathologic factors (Fig. 1). Patients with clinically higher risk factors (male and IND/LGD) were predicted to progress at a higher rate (4.8%; IQR 2-12) than patients with clinically lower risk factors (female and NDBE, 3.0%; IQR 1.8-5.1, P< 0.0001, Table 1). In NDBE female patients, TSP-9 identified 15.2% of patients as intermediate/high risk for progression with a predicted 5-year progression rate of 8.1% (IQR, 7-9) and 16.6% (IQR, 13-26), respectively, which was significantly higher than progression rates in males with IND/LGD (4.8%; IQR, 2-12) (P< 0.0001, Fig. 1B-C). The TSP-9 test identified 71.4% of IND/LGD male patients as low-risk with a predicted 5-year progression rate of 2.8% (IQR 2-4), which can enable confidence in a surveillance-only approach (Fig. 1C).
Discussion: The TSP-9 test provided significant risk stratification in clinical practice, including in patients considered to be at low risk for malignant progression based on clinicopathologic features. TSP-9 identified 15.2% of NDBE females as intermediate/high-risk for progression providing objective results to guide escalation of care with the goal of preventing EAC. The test also identified low-risk patients who can safely be managed by surveillance. Clinically impactful risk stratification by TSP-9 can allow physicians to consider risk-aligned management options with their patients to improve health outcomes.

Figure: Figure 1. TSP-9 risk-stratification results in clinically higher risk and clinically lower risk subsets of BE patients. Percentage of patients scoring TSP-9 low-, intermediate- or high-risk and predicted probability of progression to HGD/EAC within 5 years in (A) BE patients, (B) Male BE patients with the diagnosis of indefinite for dysplasia (IND), and low-grade dysplasia (LGD); (C) Female BE patients with a diagnosis of non-dysplastic BE (NDBE). Diagnoses and clinical variables were abstracted from pathology/endoscopy reports.
Disclosures:
Harshit Khara: Boston Scientific – Consultant, Speakers Bureau. Castle Biosciences – Consultant, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook Medical – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus America – Consultant, Speakers Bureau. Pentax – Consultant, Speakers Bureau.
Michael Yodice indicated no relevant financial relationships.
Nicolas Villa indicated no relevant financial relationships.
Miguel Ordonez-Castellanos indicated no relevant financial relationships.
Christian Smolko: Castle Biosciences – Employee, Stock-publicly held company(excluding mutual/index funds).
Meenakshi Arora: Castle Biosciences – Stock Options.
Rebecca J. Critchley-Thorne: Castle Biosciences – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
David Diehl: Boston Scientific – Consultant. Castle – Consultant. Laborie – Consultant. Merit Endotek – Consultant. Microtech – Consultant. Olympus – Consultant. OnePass Medical – Consultant. Pentax – Consultant. Steris – Consultant.
Harshit S. Khara, MD1, Michael Yodice, MD1, Nicolas Villa, MD2, Miguel Ordonez-Castellanos, MD3, Christian Smolko, PhD4, Meenakshi Arora, PhD4, Rebecca J. Critchley-Thorne, PhD4, David L. Diehl, MD1. P3265 - The Tissue Systems Pathology Test Objectively Risk-Stratifies Patients with Barrett’s Esophagus: A Multicenter US Clinical Experience Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
