Tuesday Poster Session
Category: Esophagus
P3266 - Deep Learning System for Differentiation of Malignant From Benign Lymph Nodes on EUS Staging of Esophageal Cancer: A Pilot Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ahmed Nadeem, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Abel Joseph, MD1, Ahmed Nadeem, MD1, David Chen, PhD1, Yi Qin, MD2, Shuaiqi Huang, PhD1, Xiaofeng Wang, PhD1, Sunguk Jang, MD2, Madhusudhan R.. Sanaka, MD2, Prabhleen Chahal, MD2, John Vargo, MD1, Siva Raja, MD2, Sudish Murthy, MD2, Amit Bhatt, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: The management of esophageal cancer (EC) is dependent on accurate pre-treatment staging. While endoscopic ultrasound (EUS) has remained the best available tool for locoregional staging and lymph node (LN) detection before surgery, the accuracy of EUS is operator dependent and low. There is limited literature on the use of deep learning systems for esophageal cancer EUS. EUS is largely dependent on identifying visual patterns and artificial intelligence using a deep learning model can offer an objective way of malignant LN detection. Therefore, we aimed to develop and validate a deep learning model to differentiate benign from malignant lymph nodes during EUS staging of esophageal cancer.
Methods: The management of esophageal cancer (EC) is dependent on accurate pre-treatment staging. While endoscopic ultrasound (EUS) has remained the best available tool for locoregional staging and lymph node (LN) detection before surgery, the accuracy of EUS is operator dependent and low. There is limited literature on the use of deep learning systems for esophageal cancer EUS. EUS is largely dependent on identifying visual patterns and artificial intelligence using a deep learning model can offer an objective way of malignant LN detection. Therefore, we aimed to develop and validate a deep learning model to differentiate benign from malignant lymph nodes during EUS staging of esophageal cancer.
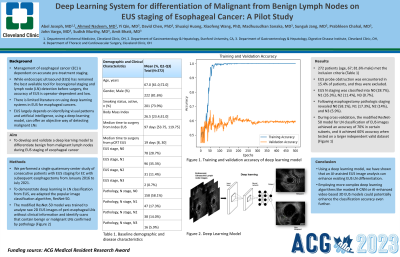
Results: 237 patients (age, 67; 81.6% male) met the inclusion criteria. Patients with EUS probe obstruction and lack of EUS images were excluded (99/336 (29.4%)). EUS N staging was classified into N0 (28.7%), N1 (35.3%), N2 (11.4%), N3 (0.7%). Following esophagectomy pathologic staging included N0 (58.1%), N1 (17.3%), N2 (14%), N3 (5.9%). During cross-validation, the modified ResNet-50 model for LN classification of EUS images achieved an accuracy of 70% in certain subsets, and it achieved 60% accuracy when tested on a larger independent valid dataset.
Discussion: Using a deep learning model, we have shown that an AI-assisted EUS image analysis can enhance existing operator-dependent EUS LN differentiation. Given the relatively small training dataset size and the limited resolution of the scans, employing more complex deep learning algorithms like masked R-CNN or AI-enhanced video-based 3D EUS models could potentially enhance the classification accuracy even further.

Disclosures:
Abel Joseph, MD1, Ahmed Nadeem, MD1, David Chen, PhD1, Yi Qin, MD2, Shuaiqi Huang, PhD1, Xiaofeng Wang, PhD1, Sunguk Jang, MD2, Madhusudhan R.. Sanaka, MD2, Prabhleen Chahal, MD2, John Vargo, MD1, Siva Raja, MD2, Sudish Murthy, MD2, Amit Bhatt, MD1. P3266 - Deep Learning System for Differentiation of Malignant From Benign Lymph Nodes on EUS Staging of Esophageal Cancer: A Pilot Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: The management of esophageal cancer (EC) is dependent on accurate pre-treatment staging. While endoscopic ultrasound (EUS) has remained the best available tool for locoregional staging and lymph node (LN) detection before surgery, the accuracy of EUS is operator dependent and low. There is limited literature on the use of deep learning systems for esophageal cancer EUS. EUS is largely dependent on identifying visual patterns and artificial intelligence using a deep learning model can offer an objective way of malignant LN detection. Therefore, we aimed to develop and validate a deep learning model to differentiate benign from malignant lymph nodes during EUS staging of esophageal cancer.
Methods: The management of esophageal cancer (EC) is dependent on accurate pre-treatment staging. While endoscopic ultrasound (EUS) has remained the best available tool for locoregional staging and lymph node (LN) detection before surgery, the accuracy of EUS is operator dependent and low. There is limited literature on the use of deep learning systems for esophageal cancer EUS. EUS is largely dependent on identifying visual patterns and artificial intelligence using a deep learning model can offer an objective way of malignant LN detection. Therefore, we aimed to develop and validate a deep learning model to differentiate benign from malignant lymph nodes during EUS staging of esophageal cancer.
Results: 237 patients (age, 67; 81.6% male) met the inclusion criteria. Patients with EUS probe obstruction and lack of EUS images were excluded (99/336 (29.4%)). EUS N staging was classified into N0 (28.7%), N1 (35.3%), N2 (11.4%), N3 (0.7%). Following esophagectomy pathologic staging included N0 (58.1%), N1 (17.3%), N2 (14%), N3 (5.9%). During cross-validation, the modified ResNet-50 model for LN classification of EUS images achieved an accuracy of 70% in certain subsets, and it achieved 60% accuracy when tested on a larger independent valid dataset.
Discussion: Using a deep learning model, we have shown that an AI-assisted EUS image analysis can enhance existing operator-dependent EUS LN differentiation. Given the relatively small training dataset size and the limited resolution of the scans, employing more complex deep learning algorithms like masked R-CNN or AI-enhanced video-based 3D EUS models could potentially enhance the classification accuracy even further.

Figure: Figure 1. Training and validation accuracy of deep learning model.
Disclosures:
Abel Joseph indicated no relevant financial relationships.
Ahmed Nadeem indicated no relevant financial relationships.
David Chen indicated no relevant financial relationships.
Yi Qin indicated no relevant financial relationships.
Shuaiqi Huang indicated no relevant financial relationships.
Xiaofeng Wang indicated no relevant financial relationships.
Sunguk Jang indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Prabhleen Chahal indicated no relevant financial relationships.
John Vargo indicated no relevant financial relationships.
Siva Raja indicated no relevant financial relationships.
Sudish Murthy indicated no relevant financial relationships.
Amit Bhatt: Boston Scientific – Consultant. Medtronic – Consultant, Intellectual Property/Patents. Steris – Consultant.
Abel Joseph, MD1, Ahmed Nadeem, MD1, David Chen, PhD1, Yi Qin, MD2, Shuaiqi Huang, PhD1, Xiaofeng Wang, PhD1, Sunguk Jang, MD2, Madhusudhan R.. Sanaka, MD2, Prabhleen Chahal, MD2, John Vargo, MD1, Siva Raja, MD2, Sudish Murthy, MD2, Amit Bhatt, MD1. P3266 - Deep Learning System for Differentiation of Malignant From Benign Lymph Nodes on EUS Staging of Esophageal Cancer: A Pilot Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
