Tuesday Poster Session
Category: Esophagus
P3268 - Do Bariatric Procedures Impact Barrett’s Esophagus and Esophageal Cancers? Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- AC
Ankit Chhoda, MD
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Mahmoud H. Abdalla, MD2, Sanam Hariri, MD3, Tatiana Andrea Rojas Zapata, MD4, Alyssa Grimshaw, MBA5, Douglas Pleskow, MD, FACG6, Violeta Popov, MD, PhD, FACG7, Erik Holzwanger, MD1
1Beth Israel Deaconess Medical Center, Boston, MA; 2AdventHealth, Tampa, FL; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 4Universidad del Norte, Cali, Valle del Cauca, Colombia; 5Yale University Libraries, West Haven, CT; 6BIDMC, Boston, MA; 7NYU Langone Health, New York, NY
Introduction: Barret’s esophagus (BE), a precursor to esophageal adenocarcinoma (EAC), has high prevalence of 0.5–2.0% & has increasing burden in the Western World. Although BE & EAC are associated with chronic reflux, their burden among bariatric population procedures is compelling domain for investigation. Among patients undergoing bariatric surgeries, we aimed to quantify the incidence & progression of BE & the overall risk of esophageal carcinogenesis.
Methods: A systematic search from Cochrane, Embase, Google Scholar, Medline, PubMed, Scopus, & Web of Science identified bariatric surgical studies with discrete endoscopic & histological findings. The outcomes of interest included: patient demographics, type of bariatric procedure (classified as Group I: Roux-en-Y Gastric Bypass; II: Sleeve Gastrectomy; III: Biliopancreatic Diversion with Duodenal Switch; IV: Adjustable Gastric Banding), pre- & post-bariatric procedural endoscopic and histological findings. The burden of BE, EAC, BE progression was described as pooled incidence[95% confidence intervals] & meta-analysis was performed using a random-effects model.
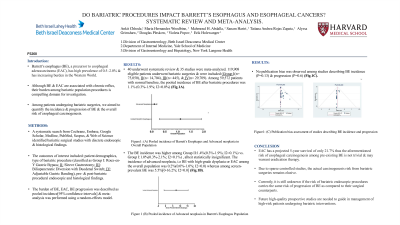
Results: 40 underwent systematic review & 35 studies were meta-analyzed. 119,908 eligible patients underwent bariatric surgeries & were included (Group I(n= 75,050), II(n= 14,704), III(n= 445), & IV(n= 29,709). Among 59,572 patients with normal baseline, the pooled incidence of BE after bariatric procedures was 1.1% (0.3%-1.9%; I2=0.0%) (Fig.1A). The BE incidence was higher among Group II:1.4%(0.3%-1.9%; I2=0.1%) vs. Group I:1.0%(0.3%-2.1%; I2=0.1%) , albeit statistically insignificant. The incidence of advanced neoplasia, i.e BE with high-grade dysplasia or EAC among the overall population was 0.2%(0.0%-1.0%; I2=0.0) whereas among screen-prevalent BE was 5.5%[0-16.2%; I2=0.0] (Fig.1B). No publication bias was observed among studies describing BE incidence (P=0.13) & progression (P=0.6) (Fig.1C).
Discussion: EAC has a projected 5-year survival of only 21.7% thus the aforementioned risk of esophageal carcinogenesis among pre-existing BE is not trivial & may warrant eradication therapy. Due to sparse controlled studies, the actual carcinogenesis risk from bariatric surgeries remains elusive. Currently, it is still unknown if the risk of bariatric endoscopic procedures carries the same risk of progression of BE as compared to their surgical counterparts. Future high-quality prospective studies are needed to guide in management of high-risk patients undergoing bariatric interventions.

Disclosures:
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Mahmoud H. Abdalla, MD2, Sanam Hariri, MD3, Tatiana Andrea Rojas Zapata, MD4, Alyssa Grimshaw, MBA5, Douglas Pleskow, MD, FACG6, Violeta Popov, MD, PhD, FACG7, Erik Holzwanger, MD1. P3268 - Do Bariatric Procedures Impact Barrett’s Esophagus and Esophageal Cancers? Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2AdventHealth, Tampa, FL; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 4Universidad del Norte, Cali, Valle del Cauca, Colombia; 5Yale University Libraries, West Haven, CT; 6BIDMC, Boston, MA; 7NYU Langone Health, New York, NY
Introduction: Barret’s esophagus (BE), a precursor to esophageal adenocarcinoma (EAC), has high prevalence of 0.5–2.0% & has increasing burden in the Western World. Although BE & EAC are associated with chronic reflux, their burden among bariatric population procedures is compelling domain for investigation. Among patients undergoing bariatric surgeries, we aimed to quantify the incidence & progression of BE & the overall risk of esophageal carcinogenesis.
Methods: A systematic search from Cochrane, Embase, Google Scholar, Medline, PubMed, Scopus, & Web of Science identified bariatric surgical studies with discrete endoscopic & histological findings. The outcomes of interest included: patient demographics, type of bariatric procedure (classified as Group I: Roux-en-Y Gastric Bypass; II: Sleeve Gastrectomy; III: Biliopancreatic Diversion with Duodenal Switch; IV: Adjustable Gastric Banding), pre- & post-bariatric procedural endoscopic and histological findings. The burden of BE, EAC, BE progression was described as pooled incidence[95% confidence intervals] & meta-analysis was performed using a random-effects model.
Results: 40 underwent systematic review & 35 studies were meta-analyzed. 119,908 eligible patients underwent bariatric surgeries & were included (Group I(n= 75,050), II(n= 14,704), III(n= 445), & IV(n= 29,709). Among 59,572 patients with normal baseline, the pooled incidence of BE after bariatric procedures was 1.1% (0.3%-1.9%; I2=0.0%) (Fig.1A). The BE incidence was higher among Group II:1.4%(0.3%-1.9%; I2=0.1%) vs. Group I:1.0%(0.3%-2.1%; I2=0.1%) , albeit statistically insignificant. The incidence of advanced neoplasia, i.e BE with high-grade dysplasia or EAC among the overall population was 0.2%(0.0%-1.0%; I2=0.0) whereas among screen-prevalent BE was 5.5%[0-16.2%; I2=0.0] (Fig.1B). No publication bias was observed among studies describing BE incidence (P=0.13) & progression (P=0.6) (Fig.1C).
Discussion: EAC has a projected 5-year survival of only 21.7% thus the aforementioned risk of esophageal carcinogenesis among pre-existing BE is not trivial & may warrant eradication therapy. Due to sparse controlled studies, the actual carcinogenesis risk from bariatric surgeries remains elusive. Currently, it is still unknown if the risk of bariatric endoscopic procedures carries the same risk of progression of BE as compared to their surgical counterparts. Future high-quality prospective studies are needed to guide in management of high-risk patients undergoing bariatric interventions.

Figure: Figure1: (A) Pooled incidence of Barrett's Esophagus and Advanced neoplasia in Overall Population (B) Pooled incidence of Advanced neoplasia in Barrett's Esophagus Population (C) Publication bias assessment of studies describing BE incidence and progression
Disclosures:
Ankit Chhoda indicated no relevant financial relationships.
Maria Hernandez Woodbine indicated no relevant financial relationships.
Mahmoud Abdalla indicated no relevant financial relationships.
Sanam Hariri indicated no relevant financial relationships.
Tatiana Andrea Rojas Zapata indicated no relevant financial relationships.
Alyssa Grimshaw indicated no relevant financial relationships.
Douglas Pleskow: Boston Scientific – Consultant. Fuji – Consultant. Olympus – Consultant.
Violeta Popov indicated no relevant financial relationships.
Erik Holzwanger indicated no relevant financial relationships.
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Mahmoud H. Abdalla, MD2, Sanam Hariri, MD3, Tatiana Andrea Rojas Zapata, MD4, Alyssa Grimshaw, MBA5, Douglas Pleskow, MD, FACG6, Violeta Popov, MD, PhD, FACG7, Erik Holzwanger, MD1. P3268 - Do Bariatric Procedures Impact Barrett’s Esophagus and Esophageal Cancers? Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
