Tuesday Poster Session
Category: Esophagus
P3273 - Impact of Hiatal Hernia on Reliability of FLIP Testing
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- JM
James Miller, MD
Wake Forest University School of Medicine
Charlotte, NC
Presenting Author(s)
James Miller, MD1, Steven Clayton, MD2
1Wake Forest University School of Medicine, Charlotte, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Hiatal hernia (HH) is a common disorder and can be diagnosed by a diversity of tests. Currently, esophagogastroduodenoscopy (EGD), manometry, and contrast studies are all recommended as useful in diagnosing hiatal hernia, with variation in the literature regarding which is the most effective. The functional lumen imaging probe (FLIP) has arisen as a useful tool in assessing esophageal physiology, and recently shown to have significant agreement with manometry in detecting HH. However, it is still unclear as to how HH physiology affects FLIP measurements. We aimed to determine if presence of hiatal hernia impacts the reliability of FLIP measurement compared to existing tests as standards.
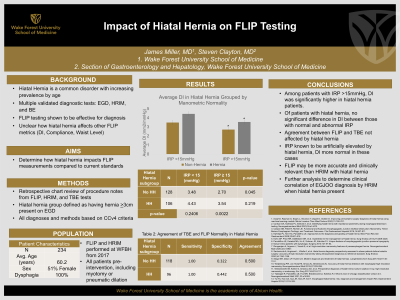
Methods: Data was collected by retrospective review of procedure notes from patients who underwent both HRIM and FLIP for work up of dysphagia. Diagnoses were based on the most updated criteria established in CCv4. Presence of hiatal hernia was determined by EGD report at time of FLIP, and patients were grouped by hernia (>3cm) or non-hernia.
Results: Agreement between overall FLIP and TBE normality determination was 50% for both the hernia and non-hernia groups (k=0.18, 0.20). Agreement between TBE normality and FLIP DI >2.8 mm2/mmHg was 64.4% in hernia group, 50.4% in non-hernia group (k=0.122, 0.052).
In the non-hernia group, average DI was 3.48 mm2/mmHg + 2.44 mm2/mmHg in patients with IRP < 15mmHg, and 2.70 mm2/mmHg + 2.58 mm2/mmHg in patients with IRP >15mmHg (p=0.045). In the hernia group, average DI was 4.43 mm2/mmHg + 2.95 mm2/mmHg in patients with IRP < 15mmHg and 3.54 mm2/mmHg + 2.34 mm2/mmHg in patients with IRP >15mmHg (p=0.219). Of patients with IRP >15mmHg, the average DI differed between hernia and non-hernia groups by a statistically significant amount between normal and pathologic range, respectively. (p=0.002).
Discussion: The hernia group had significantly higher average DI in patients with both normal and elevated IRP. Knowing that IRP can be artificially elevated by presence of hiatal hernia, DI may therefore be a more accurate assessment of lower esophageal sphincter physiology in these cases. FLIP may therefore provide a more clinically relevant measure in mechanical outlet obstruction. Hiatal hernia did not significantly influence the agreement or sensitivity of FLIP compared to TBE. This suggests that hiatal hernia did not affect DI measurement in a meaningful way.
Disclosures:
James Miller, MD1, Steven Clayton, MD2. P3273 - Impact of Hiatal Hernia on Reliability of FLIP Testing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wake Forest University School of Medicine, Charlotte, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Hiatal hernia (HH) is a common disorder and can be diagnosed by a diversity of tests. Currently, esophagogastroduodenoscopy (EGD), manometry, and contrast studies are all recommended as useful in diagnosing hiatal hernia, with variation in the literature regarding which is the most effective. The functional lumen imaging probe (FLIP) has arisen as a useful tool in assessing esophageal physiology, and recently shown to have significant agreement with manometry in detecting HH. However, it is still unclear as to how HH physiology affects FLIP measurements. We aimed to determine if presence of hiatal hernia impacts the reliability of FLIP measurement compared to existing tests as standards.
Methods: Data was collected by retrospective review of procedure notes from patients who underwent both HRIM and FLIP for work up of dysphagia. Diagnoses were based on the most updated criteria established in CCv4. Presence of hiatal hernia was determined by EGD report at time of FLIP, and patients were grouped by hernia (>3cm) or non-hernia.
Results: Agreement between overall FLIP and TBE normality determination was 50% for both the hernia and non-hernia groups (k=0.18, 0.20). Agreement between TBE normality and FLIP DI >2.8 mm2/mmHg was 64.4% in hernia group, 50.4% in non-hernia group (k=0.122, 0.052).
In the non-hernia group, average DI was 3.48 mm2/mmHg + 2.44 mm2/mmHg in patients with IRP < 15mmHg, and 2.70 mm2/mmHg + 2.58 mm2/mmHg in patients with IRP >15mmHg (p=0.045). In the hernia group, average DI was 4.43 mm2/mmHg + 2.95 mm2/mmHg in patients with IRP < 15mmHg and 3.54 mm2/mmHg + 2.34 mm2/mmHg in patients with IRP >15mmHg (p=0.219). Of patients with IRP >15mmHg, the average DI differed between hernia and non-hernia groups by a statistically significant amount between normal and pathologic range, respectively. (p=0.002).
Discussion: The hernia group had significantly higher average DI in patients with both normal and elevated IRP. Knowing that IRP can be artificially elevated by presence of hiatal hernia, DI may therefore be a more accurate assessment of lower esophageal sphincter physiology in these cases. FLIP may therefore provide a more clinically relevant measure in mechanical outlet obstruction. Hiatal hernia did not significantly influence the agreement or sensitivity of FLIP compared to TBE. This suggests that hiatal hernia did not affect DI measurement in a meaningful way.
Disclosures:
James Miller indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
James Miller, MD1, Steven Clayton, MD2. P3273 - Impact of Hiatal Hernia on Reliability of FLIP Testing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
