Tuesday Poster Session
Category: Esophagus
P3295 - A Unique Presentation of Esophageal Perforation Secondary to a Fistulizing Ventral Epidural Abscess
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Qumber Ali, BS, DO
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Qumber Ali, BS, DO, Divya Shah, BS, MD, Sally Suliman, MD
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Esophageal perforations are surgical or endoscopic emergencies often due to a spontaneous event such as trauma, foreign body ingestion, iatrogenic instrumentation, or via effort-induced injury. Retained gastric contents may enter the mediastinum causing infection, necrosis, and death. Less frequently are instances of esophageal perforation caused by insidious factors. We present a rare case of esophageal perforation secondary to a fistulizing ventral epidural abscess from retained cervical hardware.
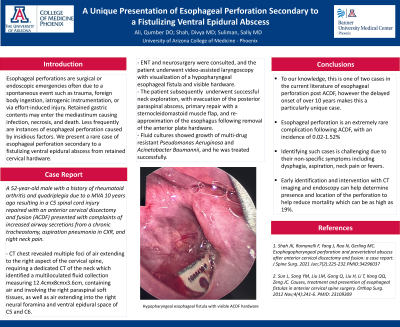
Case Description/Methods: A 52-year-old male with a history of rheumatoid arthritis and quadriplegia due to a MVA 10 years ago resulting in a C5 spinal cord injury repaired with an anterior cervical discectomy and fusion (ACDF) presented with complaints of increased airway secretions from a chronic tracheostomy, aspiration pneumonia in CXR, and right neck pain. A CT chest revealed multiple foci of air extending to the right aspect of the cervical spine, requiring a dedicated CT of the neck which identified a multiloculated fluid collection measuring 12.4cmx8cmx3.6cm, containing air and involving the right paraspinal soft tissues, as well as air extending into the right neural foramina and ventral epidural space of C5 and C6. ENT and neurosurgery were consulted, and the patient underwent video-assisted laryngoscopy with visualization of a hypopharyngeal esophageal fistula and visible hardware. He underwent successful neck exploration, with evacuation of the posterior paraspinal abscess, primary repair with a sternocleidomastoid muscle flap, and re-approximation of the esophagus following removal of the anterior plate hardware. Fluid cultures showed growth of multi-drug resistant Pseudomonas Aeurigonsa and Acinetobacter Baumannii, and he was treated successfully.
Discussion: Esophageal perforation is an extremely rare complication following ACDF, with an incidence of 0.02-1.52%. Identifying such cases is challenging due to their non-specific symptoms including dysphagia, aspiration, neck pain or fevers. Early identification and intervention with CT imaging and endoscopy can help determine presence and location of the perforation to help reduce mortality which can be as high as 19%.
To our knowledge, this is one of two cases in the current literature of esophageal perforation post ACDF, however the delayed onset of over 10 years makes this a particularly unique case highlighting the importance of high clinical suspicion and early multi-disciplinary intervention to help improve patient outcomes.

Disclosures:
Qumber Ali, BS, DO, Divya Shah, BS, MD, Sally Suliman, MD. P3295 - A Unique Presentation of Esophageal Perforation Secondary to a Fistulizing Ventral Epidural Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Esophageal perforations are surgical or endoscopic emergencies often due to a spontaneous event such as trauma, foreign body ingestion, iatrogenic instrumentation, or via effort-induced injury. Retained gastric contents may enter the mediastinum causing infection, necrosis, and death. Less frequently are instances of esophageal perforation caused by insidious factors. We present a rare case of esophageal perforation secondary to a fistulizing ventral epidural abscess from retained cervical hardware.
Case Description/Methods: A 52-year-old male with a history of rheumatoid arthritis and quadriplegia due to a MVA 10 years ago resulting in a C5 spinal cord injury repaired with an anterior cervical discectomy and fusion (ACDF) presented with complaints of increased airway secretions from a chronic tracheostomy, aspiration pneumonia in CXR, and right neck pain. A CT chest revealed multiple foci of air extending to the right aspect of the cervical spine, requiring a dedicated CT of the neck which identified a multiloculated fluid collection measuring 12.4cmx8cmx3.6cm, containing air and involving the right paraspinal soft tissues, as well as air extending into the right neural foramina and ventral epidural space of C5 and C6. ENT and neurosurgery were consulted, and the patient underwent video-assisted laryngoscopy with visualization of a hypopharyngeal esophageal fistula and visible hardware. He underwent successful neck exploration, with evacuation of the posterior paraspinal abscess, primary repair with a sternocleidomastoid muscle flap, and re-approximation of the esophagus following removal of the anterior plate hardware. Fluid cultures showed growth of multi-drug resistant Pseudomonas Aeurigonsa and Acinetobacter Baumannii, and he was treated successfully.
Discussion: Esophageal perforation is an extremely rare complication following ACDF, with an incidence of 0.02-1.52%. Identifying such cases is challenging due to their non-specific symptoms including dysphagia, aspiration, neck pain or fevers. Early identification and intervention with CT imaging and endoscopy can help determine presence and location of the perforation to help reduce mortality which can be as high as 19%.
To our knowledge, this is one of two cases in the current literature of esophageal perforation post ACDF, however the delayed onset of over 10 years makes this a particularly unique case highlighting the importance of high clinical suspicion and early multi-disciplinary intervention to help improve patient outcomes.

Figure: Hypopharyngeal esophageal fistula and visible ACDF hardware
Disclosures:
Qumber Ali indicated no relevant financial relationships.
Divya Shah indicated no relevant financial relationships.
Sally Suliman indicated no relevant financial relationships.
Qumber Ali, BS, DO, Divya Shah, BS, MD, Sally Suliman, MD. P3295 - A Unique Presentation of Esophageal Perforation Secondary to a Fistulizing Ventral Epidural Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
