Tuesday Poster Session
Category: Esophagus
P3297 - A Delayed Diagnosis of Isolated Oropharyngeal and Esophageal Pemphigus Vulgaris
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Victoria Caruso, DO
University of Massachusetts-Chan Baystate Medical Center, CT
Presenting Author(s)
Victoria Caruso, DO1, Mohammad Abdulelah, MD2, Yesenia Greeff, MD3
1University of Massachusetts-Chan Baystate Medical Center, Springfield, MA; 2Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate, Springfield, MA
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disorder that primarily affects the skin and mucous membranes, most commonly the oral and genital mucosa. While more rare, it can also involve the esophagus resulting in odynophagia and dysphagia. The role that herpes simplex virus (HSV) may play in this disorder as a trigger or result of PV has not yet been fully elucidated.
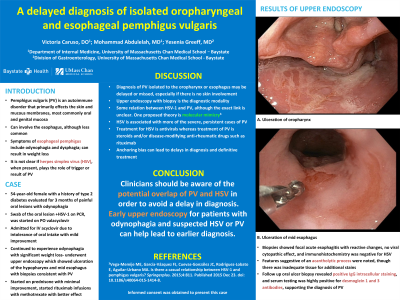
Case Description/Methods: A 54-year-old female with a history of type 2 diabetes was evaluated for three months of painful oral ulcerations and odynophagia. HSV-1 PCR swab of the oral lesion was positive so she was started on oral valacyclovir, but was admitted for intravenous acyclovir due to intolerance of oral intake. Due to her weight loss and odynophagia upper endoscopy was performed and revealed ulceration of the hypopharynx and mid esophagus (image 1). Biopsy of the mid esophagus showed focal acute esophagitis with reactive changes, no viral cytopathic effect, and immunohistochemistry was negative for HSV. Features suggestive of an acantholytic process were noted, though there was inadequate tissue for additional stains. Follow up oral ulcer biopsy revealed positive IgG intracellular staining, and serum testing was highly positive for desmoglein 1 and 3 antibodies, supporting the diagnosis of PV. The patient was started on prednisone with only minimal improvement, and is now due to start rituximab.
Discussion: Oral involvement is not uncommon in PV, and is the first sign of PV in 50% of cases. Unfortunately the diagnosis of esophageal involvement is often delayed and likely underappreaciated. The available data on the association between HSV and PV is conflicting and sparse. Some studies associate PV as a trigger for HSV, while other studies indicate that mucosal lesions facilitate viral infection. Diagnosis is ultimately made at the level of endoscopic tissue biopsy. Regardless, recommended management is antivirals for HSV and steroids or rituximab for PV. Clinicians should be aware for the potential overlap of these two conditions in order to avoid a delay in diagnosis as suffered by our patient presented here. Early upper endoscopy for patients with odynophagia and suspected HSV or PV can help lead to earlier diagnosis.

Disclosures:
Victoria Caruso, DO1, Mohammad Abdulelah, MD2, Yesenia Greeff, MD3. P3297 - A Delayed Diagnosis of Isolated Oropharyngeal and Esophageal Pemphigus Vulgaris, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Massachusetts-Chan Baystate Medical Center, Springfield, MA; 2Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate, Springfield, MA
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disorder that primarily affects the skin and mucous membranes, most commonly the oral and genital mucosa. While more rare, it can also involve the esophagus resulting in odynophagia and dysphagia. The role that herpes simplex virus (HSV) may play in this disorder as a trigger or result of PV has not yet been fully elucidated.
Case Description/Methods: A 54-year-old female with a history of type 2 diabetes was evaluated for three months of painful oral ulcerations and odynophagia. HSV-1 PCR swab of the oral lesion was positive so she was started on oral valacyclovir, but was admitted for intravenous acyclovir due to intolerance of oral intake. Due to her weight loss and odynophagia upper endoscopy was performed and revealed ulceration of the hypopharynx and mid esophagus (image 1). Biopsy of the mid esophagus showed focal acute esophagitis with reactive changes, no viral cytopathic effect, and immunohistochemistry was negative for HSV. Features suggestive of an acantholytic process were noted, though there was inadequate tissue for additional stains. Follow up oral ulcer biopsy revealed positive IgG intracellular staining, and serum testing was highly positive for desmoglein 1 and 3 antibodies, supporting the diagnosis of PV. The patient was started on prednisone with only minimal improvement, and is now due to start rituximab.
Discussion: Oral involvement is not uncommon in PV, and is the first sign of PV in 50% of cases. Unfortunately the diagnosis of esophageal involvement is often delayed and likely underappreaciated. The available data on the association between HSV and PV is conflicting and sparse. Some studies associate PV as a trigger for HSV, while other studies indicate that mucosal lesions facilitate viral infection. Diagnosis is ultimately made at the level of endoscopic tissue biopsy. Regardless, recommended management is antivirals for HSV and steroids or rituximab for PV. Clinicians should be aware for the potential overlap of these two conditions in order to avoid a delay in diagnosis as suffered by our patient presented here. Early upper endoscopy for patients with odynophagia and suspected HSV or PV can help lead to earlier diagnosis.

Figure: Image 1. Multiple shallow ulcerations in the distal esophagus
Disclosures:
Victoria Caruso indicated no relevant financial relationships.
Mohammad Abdulelah indicated no relevant financial relationships.
Yesenia Greeff indicated no relevant financial relationships.
Victoria Caruso, DO1, Mohammad Abdulelah, MD2, Yesenia Greeff, MD3. P3297 - A Delayed Diagnosis of Isolated Oropharyngeal and Esophageal Pemphigus Vulgaris, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
