Tuesday Poster Session
Category: Esophagus
P3299 - In Patients With Autoimmune Disease and Achalasia Diagnosed by HRM, FLIP Can Clarify Lower Esophageal Sphincter Function
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ambreen A. Merchant, MD
Baylor University Medical Center
Dallas, TX
Presenting Author(s)
Award: Presidential Poster Award
Ambreen A. Merchant, MD1, Ashton Ellison, MBChB2, Chanakyaram A. Reddy, MD2, Vani JA Konda, MD2, Rhonda F. Souza, MD2, Stuart J. Spechler, MD2, Anh D.. Nguyen, MD2
1Baylor University Medical Center, Dallas, TX; 2Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: While high resolution manometry (HRM) is widely regarded as the gold standard test for diagnosing esophageal motility disorders, functional luminal imaging probe (FLIP) also can provide valuable information regarding lower esophageal sphincter (LES) function. We report a series of patients with a history of autoimmune disease and HRM diagnosis of achalasia by Chicago Classification (CCv4.0), for whom subsequent evaluation by FLIP demonstrated normal EGJ opening, a finding that profoundly influenced treatment decisions.
Case Description/Methods: We reviewed medical records for patients in our Center for Esophageal Diseases with a diagnosis of autoimmune disease who also had achalasia found on HRM, and who subsequently were found to have normal EGJ opening by FLIP. Information gathered included demographics, autoimmune disease history, symptoms, treatment received and findings on esophageal function tests (esophagram, EGD, HRM and FLIP).
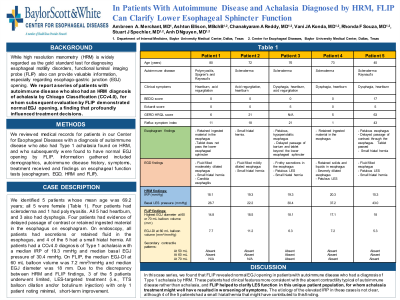
We identified 5 patients whose mean age was 69.2 years; all 5 were female (Table 1). Four patients had scleroderma and 1 had polymyositis. All 5 had heartburn, and 3 also had dysphagia. Four patients had evidence of delayed passage of contrast or retained ingested material in the esophagus on esophagram. On endoscopy, all patients had secretions or retained fluid in the esophagus, and 4 of the 5 had a small hiatal hernia. All patients had a CCv4.0 diagnosis of Type 1 achalasia with a median IRP of 19.3 mmHg and median basal EGJ pressure of 30.4 mmHg. On FLIP, the median EGJ-DI at 60 mL balloon volume was 7.2 mm2/mmHg and median EGJ diameter was 18 mm. Due to the discrepancy between HRM and FLIP findings, 3 of the 5 patients underwent limited, LES-targeted treatment (i.e., TTS balloon dilation and/or botulinum injection) with only one patient noting minimal, short-term improvement.
Discussion: In this case series, we found that FLIP revealed normal EGJ opening in patients with autoimmune disease who had a diagnosis of Type 1 achalasia by HRM. These patients had clinical features more consistent with the absent contractility typical of autoimmune disease rather than achalasia, and FLIP helped to clarify LES function in this unique patient population, for whom achalasia treatment might well have resulted in a worsening of symptoms. In our case series, 4 of 5 patients had a small hiatal hernia (noted on esophagram and/or EGD but not on HRM), which perhaps contributed to the elevated IRP on HRM.
Disclosures:
Ambreen A. Merchant, MD1, Ashton Ellison, MBChB2, Chanakyaram A. Reddy, MD2, Vani JA Konda, MD2, Rhonda F. Souza, MD2, Stuart J. Spechler, MD2, Anh D.. Nguyen, MD2. P3299 - In Patients With Autoimmune Disease and Achalasia Diagnosed by HRM, FLIP Can Clarify Lower Esophageal Sphincter Function, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Ambreen A. Merchant, MD1, Ashton Ellison, MBChB2, Chanakyaram A. Reddy, MD2, Vani JA Konda, MD2, Rhonda F. Souza, MD2, Stuart J. Spechler, MD2, Anh D.. Nguyen, MD2
1Baylor University Medical Center, Dallas, TX; 2Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: While high resolution manometry (HRM) is widely regarded as the gold standard test for diagnosing esophageal motility disorders, functional luminal imaging probe (FLIP) also can provide valuable information regarding lower esophageal sphincter (LES) function. We report a series of patients with a history of autoimmune disease and HRM diagnosis of achalasia by Chicago Classification (CCv4.0), for whom subsequent evaluation by FLIP demonstrated normal EGJ opening, a finding that profoundly influenced treatment decisions.
Case Description/Methods: We reviewed medical records for patients in our Center for Esophageal Diseases with a diagnosis of autoimmune disease who also had achalasia found on HRM, and who subsequently were found to have normal EGJ opening by FLIP. Information gathered included demographics, autoimmune disease history, symptoms, treatment received and findings on esophageal function tests (esophagram, EGD, HRM and FLIP).
We identified 5 patients whose mean age was 69.2 years; all 5 were female (Table 1). Four patients had scleroderma and 1 had polymyositis. All 5 had heartburn, and 3 also had dysphagia. Four patients had evidence of delayed passage of contrast or retained ingested material in the esophagus on esophagram. On endoscopy, all patients had secretions or retained fluid in the esophagus, and 4 of the 5 had a small hiatal hernia. All patients had a CCv4.0 diagnosis of Type 1 achalasia with a median IRP of 19.3 mmHg and median basal EGJ pressure of 30.4 mmHg. On FLIP, the median EGJ-DI at 60 mL balloon volume was 7.2 mm2/mmHg and median EGJ diameter was 18 mm. Due to the discrepancy between HRM and FLIP findings, 3 of the 5 patients underwent limited, LES-targeted treatment (i.e., TTS balloon dilation and/or botulinum injection) with only one patient noting minimal, short-term improvement.
Discussion: In this case series, we found that FLIP revealed normal EGJ opening in patients with autoimmune disease who had a diagnosis of Type 1 achalasia by HRM. These patients had clinical features more consistent with the absent contractility typical of autoimmune disease rather than achalasia, and FLIP helped to clarify LES function in this unique patient population, for whom achalasia treatment might well have resulted in a worsening of symptoms. In our case series, 4 of 5 patients had a small hiatal hernia (noted on esophagram and/or EGD but not on HRM), which perhaps contributed to the elevated IRP on HRM.
Disclosures:
Ambreen A. Merchant indicated no relevant financial relationships.
Ashton Ellison indicated no relevant financial relationships.
Chanakyaram Reddy indicated no relevant financial relationships.
Vani JA Konda: Ambu – Consultant. Castle Biosciences – Consultant. Exact Sciences – Consultant. Medtronic – Consultant.
Rhonda Souza: AstraZeneca – Consultant. Castle Biosciences – Consultant. CDx – Consultant. Ironwood Pharmaceuticals – Consultant. IsoThrive – Consultant. Phathom Pharmaceuticals – Consultant. Sanofi – Consultant.
Stuart Spechler: Castle Biosciences – Consultant. Interpace Diagnostics – Consultant. Ironwood Pharmaceuticals, Inc. – Consultant. ISOThrive, LLC – Consultant. Phathom Pharmaceuticals, Inc – Consultant. Takeda Pharmaceuticals – Consultant.
Anh Nguyen indicated no relevant financial relationships.
Ambreen A. Merchant, MD1, Ashton Ellison, MBChB2, Chanakyaram A. Reddy, MD2, Vani JA Konda, MD2, Rhonda F. Souza, MD2, Stuart J. Spechler, MD2, Anh D.. Nguyen, MD2. P3299 - In Patients With Autoimmune Disease and Achalasia Diagnosed by HRM, FLIP Can Clarify Lower Esophageal Sphincter Function, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


