Tuesday Poster Session
Category: Esophagus
P3301 - Dysphagia, Cough, and Cavitary Lung Lesions: Tuberculosis, or Is It?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kevin Kadado, DO
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Kevin Kadado, DO1, Stephanie J. Melquist, MD, MPH1, Mahmoud Mahdi, MD1, Rajeev Seecheran, MD1, Kyle Rowe, MD1, Mohammad El-Zein, MD2, William J.. Salyers, MD, MPH1
1University of Kansas School of Medicine, Wichita, KS; 2Ascension Medical Group Via Christi, Wichita, KS
Introduction: Dysphagia lusoria, first documented in 1787, remains relatively obscure in medical literature. It’s true epidemiology is unknown as it is usually asymptomatic and found incidentally. Albeit rare, the most common presenting symptom is dysphagia. Other reported symptoms include cough and chest pain. We present a compelling case of a woman thought to have tuberculosis (TB), instead was found to have dysphagia lusoria with cavitary pneumonia and cachexia.
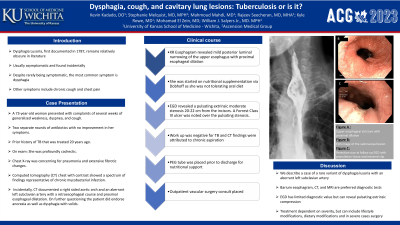
Case Description/Methods: A 73-year-old woman presented with complaints of several weeks of generalized weakness, dyspnea, and cough. During this time, the patient received two separate rounds of antibiotics with no improvement in her symptoms. Of note, the patient had a prior history of TB that was treated 20 years ago. She was profoundly cachectic. Chest X-ray was concerning for pneumonia and extensive fibrotic changes. Computed tomography (CT) chest with contrast showed a spectrum of findings representative of chronic mycobacterial infection. Incidentally, CT documented a right sided aortic arch and an aberrant left subclavian artery with a retroesophageal course and proximal esophageal dilatation. On further questioning she endorsed anorexia as well as dysphagia with solids. Barium esophagram revealed mild posterior luminal narrowing of the upper esophagus with proximal dilation. She was started on nutritional support via Dobhoff tube. Esophagogastroduodenoscopy (EGD) revealed a pulsating extrinsic moderate stenosis at 20-22 cm from the incisors (Figures A, B). A Forrest class III ulcer was noted over the pulsating stenosis (Figures C, D). No biopsies were obtained, given concerns of an underlying artery. Work up was negative for TB and the CT findings were attributed to chronic aspiration. PEG tube was placed prior to discharge for nutritional support and outpatient vascular surgery follow up was scheduled.
Discussion: Our case presents a rare variant of dysphagia lusoria, specifically an aberrant left subclavian artery with a retroesophageal course. Barium esophagram and CT and Magnetic resonance imaging are the preferred diagnostic tests. EGD has limited diagnostic value but can occasionally reveal pulsating extrinsic compression, as documented in our case. EGD was performed to exclude malignancy as a cause of luminal narrowing and place PEG. Treatment options depend on symptom severity, with options including but not limited to, lifestyle changes and dietary modifications. In severe cases, surgery is needed to correct the vascular anomaly.

Disclosures:
Kevin Kadado, DO1, Stephanie J. Melquist, MD, MPH1, Mahmoud Mahdi, MD1, Rajeev Seecheran, MD1, Kyle Rowe, MD1, Mohammad El-Zein, MD2, William J.. Salyers, MD, MPH1. P3301 - Dysphagia, Cough, and Cavitary Lung Lesions: Tuberculosis, or Is It?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Ascension Medical Group Via Christi, Wichita, KS
Introduction: Dysphagia lusoria, first documented in 1787, remains relatively obscure in medical literature. It’s true epidemiology is unknown as it is usually asymptomatic and found incidentally. Albeit rare, the most common presenting symptom is dysphagia. Other reported symptoms include cough and chest pain. We present a compelling case of a woman thought to have tuberculosis (TB), instead was found to have dysphagia lusoria with cavitary pneumonia and cachexia.
Case Description/Methods: A 73-year-old woman presented with complaints of several weeks of generalized weakness, dyspnea, and cough. During this time, the patient received two separate rounds of antibiotics with no improvement in her symptoms. Of note, the patient had a prior history of TB that was treated 20 years ago. She was profoundly cachectic. Chest X-ray was concerning for pneumonia and extensive fibrotic changes. Computed tomography (CT) chest with contrast showed a spectrum of findings representative of chronic mycobacterial infection. Incidentally, CT documented a right sided aortic arch and an aberrant left subclavian artery with a retroesophageal course and proximal esophageal dilatation. On further questioning she endorsed anorexia as well as dysphagia with solids. Barium esophagram revealed mild posterior luminal narrowing of the upper esophagus with proximal dilation. She was started on nutritional support via Dobhoff tube. Esophagogastroduodenoscopy (EGD) revealed a pulsating extrinsic moderate stenosis at 20-22 cm from the incisors (Figures A, B). A Forrest class III ulcer was noted over the pulsating stenosis (Figures C, D). No biopsies were obtained, given concerns of an underlying artery. Work up was negative for TB and the CT findings were attributed to chronic aspiration. PEG tube was placed prior to discharge for nutritional support and outpatient vascular surgery follow up was scheduled.
Discussion: Our case presents a rare variant of dysphagia lusoria, specifically an aberrant left subclavian artery with a retroesophageal course. Barium esophagram and CT and Magnetic resonance imaging are the preferred diagnostic tests. EGD has limited diagnostic value but can occasionally reveal pulsating extrinsic compression, as documented in our case. EGD was performed to exclude malignancy as a cause of luminal narrowing and place PEG. Treatment options depend on symptom severity, with options including but not limited to, lifestyle changes and dietary modifications. In severe cases, surgery is needed to correct the vascular anomaly.

Figure: Images A and B show EGD finding of moderate stenosis of the distal esophagus secondary to aberrant left subclavian artery with retroesophageal course. Images C and D show a Forrest class III ulcer noted over the area of stenosis.
Disclosures:
Kevin Kadado indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Rajeev Seecheran indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
Mohammad El-Zein indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Kevin Kadado, DO1, Stephanie J. Melquist, MD, MPH1, Mahmoud Mahdi, MD1, Rajeev Seecheran, MD1, Kyle Rowe, MD1, Mohammad El-Zein, MD2, William J.. Salyers, MD, MPH1. P3301 - Dysphagia, Cough, and Cavitary Lung Lesions: Tuberculosis, or Is It?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
