Tuesday Poster Session
Category: Esophagus
P3308 - Segmental Esophageal Spasm Associated with Diverticulosis (SESAD)
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AH
Amit Hudgi, MBBS
Medical College of Georgia at Augusta University
Augusta, Georgia
Presenting Author(s)
Amit Hudgi, MBBS, Dhanush Shimoga, MBBS, Amol Sharma, MD, MS, FACG
Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Esophageal motility disorders often co-exist with epiphrenic diverticula. Here, we present an unique case of segmental spasm in the esophagus only proximal to an epiphrenic diverticulum without co-existing esophagogastric junction (EGJ) outlet obstruction.
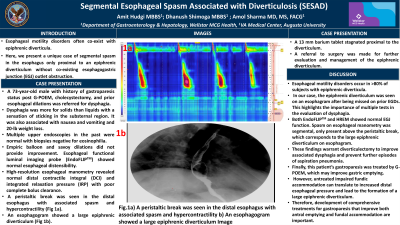
Case Description/Methods: A 73-year-old male with history of gastroparesis status post G-POEM, cholecystectomy, and prior esophageal dilations was referred for dysphagia. Dysphagia was greater for solids than liquids with a sensation of sticking in the substernal region. Dysphagia was also associated with nausea and vomiting and 20-lb weight loss. Physical examination was unremarkable. Multiple upper endoscopies in the past were normal with distal and proximal biopsies negative for eosinophilia. Empiric balloon and savoy dilations did not provide improvement in his dysphagia. Esophageal functional luminal imaging probe (EndoFLIPTM) showed normal esophageal distensibility. High-resolution esophageal manometry revealed normal distal contractile integral (DCI) and integrated relaxation pressure (IRP) with poor complete bolus clearance. A peristaltic break was seen in the distal esophagus with associated spasm and hypercontractility (Fig 1a). An esophagogram showed a large epiphrenic diverticulum (Fig 1b). A 13 mm barium tablet stagnated proximal to the diverticulum. A referral to surgery was made for further evaluation and management of the epiphrenic diverticulum.
Discussion: Esophageal motility disorders occur in >80% of subjects with epiphrenic diverticula. In our case, the epiphrenic diverticulum was seen on an esophagram after being missed on prior EGDs. This highlights the importance of multiple tests in the evaluation of dysphagia. Both EndoFLIPTM and HREM showed normal EGJ function. Spasm on esophageal manometry was segmental, only present above the peristaltic break, which corresponds to the large epiphrenic diverticulum on esophagram. These findings warrant diverticulectomy to improve associated dysphagia and prevent further episodes of aspiration pneumonia. Finally, this patient’s gastroparesis was treated by G-POEM, which may improve gastric emptying. However, untreated impaired fundic accommodation can translate to increased distal esophageal pressure and lead to the formation of a large epiphrenic diverticulum. Therefore, development of comprehensive treatments for gastroparesis that improve both antral emptying and fundal accommodation are important.

Disclosures:
Amit Hudgi, MBBS, Dhanush Shimoga, MBBS, Amol Sharma, MD, MS, FACG. P3308 - Segmental Esophageal Spasm Associated with Diverticulosis (SESAD), ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Esophageal motility disorders often co-exist with epiphrenic diverticula. Here, we present an unique case of segmental spasm in the esophagus only proximal to an epiphrenic diverticulum without co-existing esophagogastric junction (EGJ) outlet obstruction.
Case Description/Methods: A 73-year-old male with history of gastroparesis status post G-POEM, cholecystectomy, and prior esophageal dilations was referred for dysphagia. Dysphagia was greater for solids than liquids with a sensation of sticking in the substernal region. Dysphagia was also associated with nausea and vomiting and 20-lb weight loss. Physical examination was unremarkable. Multiple upper endoscopies in the past were normal with distal and proximal biopsies negative for eosinophilia. Empiric balloon and savoy dilations did not provide improvement in his dysphagia. Esophageal functional luminal imaging probe (EndoFLIPTM) showed normal esophageal distensibility. High-resolution esophageal manometry revealed normal distal contractile integral (DCI) and integrated relaxation pressure (IRP) with poor complete bolus clearance. A peristaltic break was seen in the distal esophagus with associated spasm and hypercontractility (Fig 1a). An esophagogram showed a large epiphrenic diverticulum (Fig 1b). A 13 mm barium tablet stagnated proximal to the diverticulum. A referral to surgery was made for further evaluation and management of the epiphrenic diverticulum.
Discussion: Esophageal motility disorders occur in >80% of subjects with epiphrenic diverticula. In our case, the epiphrenic diverticulum was seen on an esophagram after being missed on prior EGDs. This highlights the importance of multiple tests in the evaluation of dysphagia. Both EndoFLIPTM and HREM showed normal EGJ function. Spasm on esophageal manometry was segmental, only present above the peristaltic break, which corresponds to the large epiphrenic diverticulum on esophagram. These findings warrant diverticulectomy to improve associated dysphagia and prevent further episodes of aspiration pneumonia. Finally, this patient’s gastroparesis was treated by G-POEM, which may improve gastric emptying. However, untreated impaired fundic accommodation can translate to increased distal esophageal pressure and lead to the formation of a large epiphrenic diverticulum. Therefore, development of comprehensive treatments for gastroparesis that improve both antral emptying and fundal accommodation are important.

Figure: Fig.1a) A peristaltic break was seen in the distal esophagus with associated spasm and hypercontractility
Fig 1b) An esophagogram showed a large epiphrenic diverticulum
Fig 1b) An esophagogram showed a large epiphrenic diverticulum
Disclosures:
Amit Hudgi indicated no relevant financial relationships.
Dhanush Shimoga indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Amit Hudgi, MBBS, Dhanush Shimoga, MBBS, Amol Sharma, MD, MS, FACG. P3308 - Segmental Esophageal Spasm Associated with Diverticulosis (SESAD), ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
