Tuesday Poster Session
Category: Esophagus
P3315 - A Candid Case of Black Esophagus
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Salman Ansari, MD
University of Iowa Hospitals & Clinics
Iowa City, IA
Presenting Author(s)
Mohammad S. Ansari, MD, Ahmed Elkafrawy, MD, Amer Elsayed, MD
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: A 30 year old male with a history of alcohol use disorder, tobacco and marijuana use presented to the hospital with an episode of hematemesis. Ten days prior, he had an esophagogastroduodenoscopy (EGD) after being admitted with melena and ascites which revealed three large columns of varices, one of which had a red wale sign. He underwent successful band ligation and was discharged with antibiotics for spontaneous bacterial peritonitis prophylaxis. During his admission he was also found to have alcoholic hepatitis with a total bilirubin of 21 mg/dL and started on 40 mg of prednisolone daily.
Case Description/Methods: On admission, the patient complained of sudden onset black tarry stools followed by bloody emesis. His temperature was 99.7 F, with a heart rate of 116 per minute, blood pressure 120/80 mmHg, with a respiratory rate of 22 per minute and oxygen saturation of 99% on room air. On exam the patient was alert, tachycardic with a regular rhythm, had clear lung sounds and a soft non-tender and non-distended abdomen.
His complete blood count revealed a white blood cell count of 38 K/mm3, a hemoglobin of 7 g/dL which was 8 g/dL on discharge the prior week, and a platelet count of 332 K/mm3. His liver enzymes showed a total bilirubin of 8 mg/dL, AST of 68 U/L and ALT of 72 U/L. His INR was 1.6.
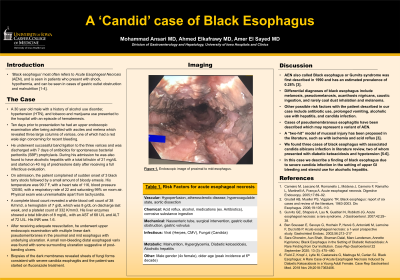
After adequate resuscitation, he underwent EGD with multiple linear dark pseudomembranes in the proximal and mid esophagus with underlying ulceration. Biopsies of the dark membranes revealed sheets of fungi forms consistent with candida and the patient was started on fluconazole.
Discussion: Black esophagus often refers to acute esophageal necrosis (AEN), and is seen in patients presenting with shock, hypothermia, and can be seen in cases of gastric outlet obstruction and malnutrition.
Differential diagnoses include melanosis, pseudomelanosis, caustic ingestion, and rarely coal dust inhalation and melanoma. Other risks include antibiotic use, prolonged vomiting, and alcoholic hepatitis. Cases of pseudomembranous esophagitis have been described which may represent a variant of AEN. A “two-hit” model of mucosal injury has been proposed in the literature. We found three cases of black esophagus with associated candida albicans infection, two of whom presented with diabetic ketoacidosis and hypotension. In this case we describe a finding of black esophagus due to severe candida infection in the setting of upper GI bleeding and steroid use for alcoholic hepatitis.

Disclosures:
Mohammad S. Ansari, MD, Ahmed Elkafrawy, MD, Amer Elsayed, MD. P3315 - A Candid Case of Black Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: A 30 year old male with a history of alcohol use disorder, tobacco and marijuana use presented to the hospital with an episode of hematemesis. Ten days prior, he had an esophagogastroduodenoscopy (EGD) after being admitted with melena and ascites which revealed three large columns of varices, one of which had a red wale sign. He underwent successful band ligation and was discharged with antibiotics for spontaneous bacterial peritonitis prophylaxis. During his admission he was also found to have alcoholic hepatitis with a total bilirubin of 21 mg/dL and started on 40 mg of prednisolone daily.
Case Description/Methods: On admission, the patient complained of sudden onset black tarry stools followed by bloody emesis. His temperature was 99.7 F, with a heart rate of 116 per minute, blood pressure 120/80 mmHg, with a respiratory rate of 22 per minute and oxygen saturation of 99% on room air. On exam the patient was alert, tachycardic with a regular rhythm, had clear lung sounds and a soft non-tender and non-distended abdomen.
His complete blood count revealed a white blood cell count of 38 K/mm3, a hemoglobin of 7 g/dL which was 8 g/dL on discharge the prior week, and a platelet count of 332 K/mm3. His liver enzymes showed a total bilirubin of 8 mg/dL, AST of 68 U/L and ALT of 72 U/L. His INR was 1.6.
After adequate resuscitation, he underwent EGD with multiple linear dark pseudomembranes in the proximal and mid esophagus with underlying ulceration. Biopsies of the dark membranes revealed sheets of fungi forms consistent with candida and the patient was started on fluconazole.
Discussion: Black esophagus often refers to acute esophageal necrosis (AEN), and is seen in patients presenting with shock, hypothermia, and can be seen in cases of gastric outlet obstruction and malnutrition.
Differential diagnoses include melanosis, pseudomelanosis, caustic ingestion, and rarely coal dust inhalation and melanoma. Other risks include antibiotic use, prolonged vomiting, and alcoholic hepatitis. Cases of pseudomembranous esophagitis have been described which may represent a variant of AEN. A “two-hit” model of mucosal injury has been proposed in the literature. We found three cases of black esophagus with associated candida albicans infection, two of whom presented with diabetic ketoacidosis and hypotension. In this case we describe a finding of black esophagus due to severe candida infection in the setting of upper GI bleeding and steroid use for alcoholic hepatitis.

Figure: Pseudomembranous black esophagus
Disclosures:
Mohammad Ansari indicated no relevant financial relationships.
Ahmed Elkafrawy indicated no relevant financial relationships.
Amer Elsayed indicated no relevant financial relationships.
Mohammad S. Ansari, MD, Ahmed Elkafrawy, MD, Amer Elsayed, MD. P3315 - A Candid Case of Black Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
