Tuesday Poster Session
Category: Esophagus
P3317 - Esophageal Lichen Planus Managed With Serial Esophagogastroduodenoscopy Dilations
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Tyrell Daniel, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Tyrell Daniel, MD1, Jordan Gladys-Oryhon, DO2, Harmeet Kharoud, MD2, Raktima Goswami, MD2
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: Lichen planus is a mucocutaneous condition that typically affects the skin or mouth. Esophageal involvement is rare but when present, dysphagia is seen. Here we present a case of Esophageal Lichen planus (ELP) refractory to medical therapy treated with serial EGD dilations.
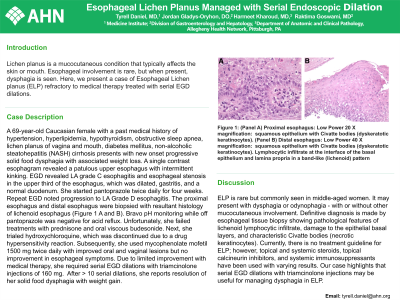
Case Description/Methods: A 69-year-old Caucasian female with a past medical history of hypertension, hyperlipidemia, hypothyroidism, obstructive sleep apnea, lichen planus of vagina and mouth, diabetes mellitus, non-alcoholic steatohepatitis (NASH) cirrhosis presented to the clinic with a chief complaint of new onset progressive dysphagia to solid food with associated weight loss. A single contrast esophagram revealed a patulous upper esophagus with intermittent kinking. EGD revealed LA grade C esophagitis and esophageal stenosis in the upper third of the esophagus, which was dilated, gastritis, and a normal duodenum. She started pantoprazole twice daily for 4 weeks. Repeat EGD noted progression to LA Grade D esophagitis. The proximal esophagus and distal esophagus were biopsied with resultant histology of lichenoid esophagus (Figure 1 A and B). Bravo pH monitoring while off pantoprazole was negative for acid reflux. Unfortunately, she failed treatments with prednisone and oral viscous budesonide. Next, she tried hydroxychloroquine, but it was discontinued because of a drug hypersensitivity reaction. Subsequently, she used mycophenolate mofetil 1500 mg twice daily with improvement in oral and vaginal lesions but no improvement in esophageal symptoms. Due to limited improvement with medications, she has required serial EGD dilations with triamcinolone injections of 160 mg for strictures that have been subsequently found throughout the esophagus. After > 10 serial dilations, she reports resolution of her dysphagia with weight gain.
Discussion: ELP is rare but commonly seen in middle aged women. It may present with dysphagia or odynophagia - with or without other mucocutaneous involvement. Definitive diagnosis is made by esophageal tissue biopsy showing pathological features of lichenoid lymphocytic infiltrate, damage to the epithelial basal layers and characteristic Civatte bodies (necrotic keratinocytes). Currently, there is no treatment guideline for ELP however topical and systemic steroids, topical calcineurin inhibitors, systemic immunosuppressants have been used with varying results. Our case highlights that serial EGD dilations with triamcinolone injections may be useful for managing dysphagia in ELP.

Disclosures:
Tyrell Daniel, MD1, Jordan Gladys-Oryhon, DO2, Harmeet Kharoud, MD2, Raktima Goswami, MD2. P3317 - Esophageal Lichen Planus Managed With Serial Esophagogastroduodenoscopy Dilations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: Lichen planus is a mucocutaneous condition that typically affects the skin or mouth. Esophageal involvement is rare but when present, dysphagia is seen. Here we present a case of Esophageal Lichen planus (ELP) refractory to medical therapy treated with serial EGD dilations.
Case Description/Methods: A 69-year-old Caucasian female with a past medical history of hypertension, hyperlipidemia, hypothyroidism, obstructive sleep apnea, lichen planus of vagina and mouth, diabetes mellitus, non-alcoholic steatohepatitis (NASH) cirrhosis presented to the clinic with a chief complaint of new onset progressive dysphagia to solid food with associated weight loss. A single contrast esophagram revealed a patulous upper esophagus with intermittent kinking. EGD revealed LA grade C esophagitis and esophageal stenosis in the upper third of the esophagus, which was dilated, gastritis, and a normal duodenum. She started pantoprazole twice daily for 4 weeks. Repeat EGD noted progression to LA Grade D esophagitis. The proximal esophagus and distal esophagus were biopsied with resultant histology of lichenoid esophagus (Figure 1 A and B). Bravo pH monitoring while off pantoprazole was negative for acid reflux. Unfortunately, she failed treatments with prednisone and oral viscous budesonide. Next, she tried hydroxychloroquine, but it was discontinued because of a drug hypersensitivity reaction. Subsequently, she used mycophenolate mofetil 1500 mg twice daily with improvement in oral and vaginal lesions but no improvement in esophageal symptoms. Due to limited improvement with medications, she has required serial EGD dilations with triamcinolone injections of 160 mg for strictures that have been subsequently found throughout the esophagus. After > 10 serial dilations, she reports resolution of her dysphagia with weight gain.
Discussion: ELP is rare but commonly seen in middle aged women. It may present with dysphagia or odynophagia - with or without other mucocutaneous involvement. Definitive diagnosis is made by esophageal tissue biopsy showing pathological features of lichenoid lymphocytic infiltrate, damage to the epithelial basal layers and characteristic Civatte bodies (necrotic keratinocytes). Currently, there is no treatment guideline for ELP however topical and systemic steroids, topical calcineurin inhibitors, systemic immunosuppressants have been used with varying results. Our case highlights that serial EGD dilations with triamcinolone injections may be useful for managing dysphagia in ELP.

Figure: Figure 1: (Panel A) Proximal esophagus: Low Power 20 X magnification: Proximal esophagus: squamous epithelium with Civatte bodies (dyskeratotic keratinocytes). (Panel B) Distal esophagus: Low Power 40 X magnification: Distal esophagus: squamous epithelium with Civatte bodies (dyskeratotic keratinocytes). Lymphocytic infiltrate at the interface of the basal epithelium and lamina propria in a band-like (lichenoid) pattern
Disclosures:
Tyrell Daniel indicated no relevant financial relationships.
Jordan Gladys-Oryhon indicated no relevant financial relationships.
Harmeet Kharoud indicated no relevant financial relationships.
Raktima Goswami indicated no relevant financial relationships.
Tyrell Daniel, MD1, Jordan Gladys-Oryhon, DO2, Harmeet Kharoud, MD2, Raktima Goswami, MD2. P3317 - Esophageal Lichen Planus Managed With Serial Esophagogastroduodenoscopy Dilations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
