Tuesday Poster Session
Category: Esophagus
P3325 - Missed Diagnosis? The Deceptiveness of Pseudoachalasia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Devanshi Kajal, MD
East Carolina University
Greenville, NC
Presenting Author(s)
Devanshi Kajal, MD1, Mary-Jane Williams, MD2
1East Carolina University, Greenville, NC; 2East Carolina University Brody School of Medicine, Greenville, NC
Introduction: Pseudoachalasia is a rare disorder and is often indistinguishable from primary achalasia. It is usually associated with malignancy when it occurs in the elderly. We describe a case of chronic pseudoachalasia due to esophageal adenocarcinoma despite negative endoscopies and imaging.
Case Description/Methods: A 53 y old female with history of chronic dysphagia, recurrent acute pancreatitis, acute cholecystitis s/p laparoscopic cholecystectomy, was referred to our institution for repeat endoscopic ultrasound (EUS) after a failed peroral endoscopic myotomy (POEM) due to scarring and inability to pass the scope into the stomach. Initial gastric biopsy results from an upper endoscopy showed gastritis. Prior EUS showed a cystic lesion in the pancreatic tail suggestive of benign post inflammatory changes. Barium swallow was suggestive of achalasia, as was esophageal manometry. POEM was attempted which was unsuccessful due to scarring, hence a gastrojejunostomy tube was placed to aid nutrition. Due to no improvement in symptoms, Heller’s myotomy was planned but after a subsequent visit to the emergency department showed a new pancreatic lesion, the procedure was cancelled, and an EGD/EUS was recommended, hence the referral. Significant stenosis was noted at the lower esophageal sphincter during endoscopy precluding the use of a regular-sized scope. After using a small diameter scope, a mass was identified at the lower esophageal sphincter and the cardia, which was biopsied. The biopsy showed esophageal adenocarcinoma. Tumor markers CEA and CA19-9 were elevated. The patient was started on chemotherapy but despite multiple cycles, her cancer progressed, metastasized, and the decision was made to transition her to hospice. She passed away a few months later.
Discussion: Pseudoachalasia should be managed with a high index of suspicion for malignancy regardless of the age at diagnosis. It usually has a more rapid progression than idiopathic achalasia which necessitates its timely detection and management. Patients should undergo upper endoscopy with biopsies of any abnormal findings.

Disclosures:
Devanshi Kajal, MD1, Mary-Jane Williams, MD2. P3325 - Missed Diagnosis? The Deceptiveness of Pseudoachalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1East Carolina University, Greenville, NC; 2East Carolina University Brody School of Medicine, Greenville, NC
Introduction: Pseudoachalasia is a rare disorder and is often indistinguishable from primary achalasia. It is usually associated with malignancy when it occurs in the elderly. We describe a case of chronic pseudoachalasia due to esophageal adenocarcinoma despite negative endoscopies and imaging.
Case Description/Methods: A 53 y old female with history of chronic dysphagia, recurrent acute pancreatitis, acute cholecystitis s/p laparoscopic cholecystectomy, was referred to our institution for repeat endoscopic ultrasound (EUS) after a failed peroral endoscopic myotomy (POEM) due to scarring and inability to pass the scope into the stomach. Initial gastric biopsy results from an upper endoscopy showed gastritis. Prior EUS showed a cystic lesion in the pancreatic tail suggestive of benign post inflammatory changes. Barium swallow was suggestive of achalasia, as was esophageal manometry. POEM was attempted which was unsuccessful due to scarring, hence a gastrojejunostomy tube was placed to aid nutrition. Due to no improvement in symptoms, Heller’s myotomy was planned but after a subsequent visit to the emergency department showed a new pancreatic lesion, the procedure was cancelled, and an EGD/EUS was recommended, hence the referral. Significant stenosis was noted at the lower esophageal sphincter during endoscopy precluding the use of a regular-sized scope. After using a small diameter scope, a mass was identified at the lower esophageal sphincter and the cardia, which was biopsied. The biopsy showed esophageal adenocarcinoma. Tumor markers CEA and CA19-9 were elevated. The patient was started on chemotherapy but despite multiple cycles, her cancer progressed, metastasized, and the decision was made to transition her to hospice. She passed away a few months later.
Discussion: Pseudoachalasia should be managed with a high index of suspicion for malignancy regardless of the age at diagnosis. It usually has a more rapid progression than idiopathic achalasia which necessitates its timely detection and management. Patients should undergo upper endoscopy with biopsies of any abnormal findings.

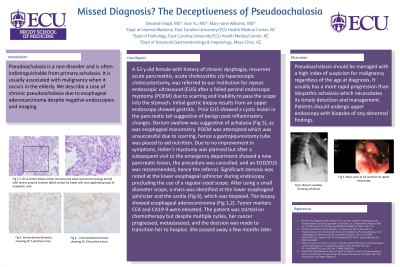
Figure: Achalasia on barium swallow and gastric cardia mass seen on endoscopy
Disclosures:
Devanshi Kajal indicated no relevant financial relationships.
Mary-Jane Williams indicated no relevant financial relationships.
Devanshi Kajal, MD1, Mary-Jane Williams, MD2. P3325 - Missed Diagnosis? The Deceptiveness of Pseudoachalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
