Tuesday Poster Session
Category: Esophagus
P3327 - “Snake-skin” Shedding Appearance of Mucosa in a Case of Esophagitis Dissecans Superficialis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Ifrah Fatima, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Ifrah Fatima, MD1, Abbas Bader, 2, Noor Hassan, MD1, Mir Zulqarnain, DO1, Pawel Szurnicki, MD3
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City, Kansas City, MO; 3Saint Luke's Hospital, Kansas City, MO
Introduction: Esophagitis Dissecans Superficialis (EDS) is a rare and benign endoscopic finding of sloughing of large fragments of esophageal mucosa. Its etiology is unknown but it has been associated with medications like bisphosphonates, NSAIDs, hot beverages, chemical irritants, autoimmune bullous diseases.
Case Description/Methods: An 81-year-old female with a past medical history of hypertension, hyperlipidemia, gastro-esophageal reflux disease, atrial fibrillation on apixaban, and Parkinson’s disease was admitted for pneumonia and hypoxemic respiratory failure. She was started on antibiotics but later had a fall from her hospital bed and developed temporal subdural hematoma. Apixaban was discontinued,
She deteriorated with worsening oxygen requirements and had 3 episodes of dark tarry stools with hemoglobin drop from 13g/dL to 9g/dL, tachycardia, and hypotension requiring ICU transfer.
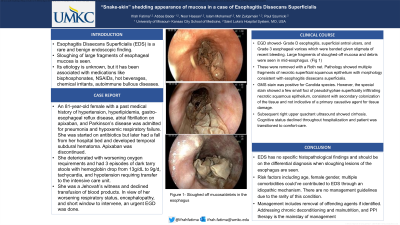
She was a Jehovah’s witness and declined transfusion of blood products. In view of her worsening respiratory status, encephalopathy, and short window to intervene, an urgent EGD was done and showed- Grade D esophagitis, antral ulcers, and Grade 3 esophageal varices with stigmata of recent bleeding which were banded. Large fragments of sloughed-off mucosa and debris were seen in mid-esophagus. (Fig 1) These were removed with a Roth net. Pathology showed multiple fragments of necrotic superficial squamous epithelium with morphology consistent with esophagitis dissecans superficialis. GMS stain was positive for Candida species. However, the special stain showed a few small foci of pseudohyphae superficially infiltrating necrotic squamous epithelium, consistent with secondary colonization of the tissue and not indicative of a primary causative agent for tissue damage.
Subsequent right upper quadrant ultrasound showed cirrhosis. Cognitive status declined throughout hospitalization and patient was transitioned to comfort-care.
Discussion: EDS has no specific histopathological findings and should be on the differential diagnosis when sloughing lesions of the esophagus are seen. Risk factors including age, female gender, multiple comorbidities could’ve contributed to EDS through an idiopathic mechanism. There are no management guidelines due to the rarity of this condition. Management includes the removal of offending agents if identified. Addressing chronic deconditioning and malnutrition, and PPI therapy has been known to show positive outcomes and improvement in symptoms.

Disclosures:
Ifrah Fatima, MD1, Abbas Bader, 2, Noor Hassan, MD1, Mir Zulqarnain, DO1, Pawel Szurnicki, MD3. P3327 - “Snake-skin” Shedding Appearance of Mucosa in a Case of Esophagitis Dissecans Superficialis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City, Kansas City, MO; 3Saint Luke's Hospital, Kansas City, MO
Introduction: Esophagitis Dissecans Superficialis (EDS) is a rare and benign endoscopic finding of sloughing of large fragments of esophageal mucosa. Its etiology is unknown but it has been associated with medications like bisphosphonates, NSAIDs, hot beverages, chemical irritants, autoimmune bullous diseases.
Case Description/Methods: An 81-year-old female with a past medical history of hypertension, hyperlipidemia, gastro-esophageal reflux disease, atrial fibrillation on apixaban, and Parkinson’s disease was admitted for pneumonia and hypoxemic respiratory failure. She was started on antibiotics but later had a fall from her hospital bed and developed temporal subdural hematoma. Apixaban was discontinued,
She deteriorated with worsening oxygen requirements and had 3 episodes of dark tarry stools with hemoglobin drop from 13g/dL to 9g/dL, tachycardia, and hypotension requiring ICU transfer.
She was a Jehovah’s witness and declined transfusion of blood products. In view of her worsening respiratory status, encephalopathy, and short window to intervene, an urgent EGD was done and showed- Grade D esophagitis, antral ulcers, and Grade 3 esophageal varices with stigmata of recent bleeding which were banded. Large fragments of sloughed-off mucosa and debris were seen in mid-esophagus. (Fig 1) These were removed with a Roth net. Pathology showed multiple fragments of necrotic superficial squamous epithelium with morphology consistent with esophagitis dissecans superficialis. GMS stain was positive for Candida species. However, the special stain showed a few small foci of pseudohyphae superficially infiltrating necrotic squamous epithelium, consistent with secondary colonization of the tissue and not indicative of a primary causative agent for tissue damage.
Subsequent right upper quadrant ultrasound showed cirrhosis. Cognitive status declined throughout hospitalization and patient was transitioned to comfort-care.
Discussion: EDS has no specific histopathological findings and should be on the differential diagnosis when sloughing lesions of the esophagus are seen. Risk factors including age, female gender, multiple comorbidities could’ve contributed to EDS through an idiopathic mechanism. There are no management guidelines due to the rarity of this condition. Management includes the removal of offending agents if identified. Addressing chronic deconditioning and malnutrition, and PPI therapy has been known to show positive outcomes and improvement in symptoms.

Figure: Figure 1- Sloughed off mucosa/debris in the esophagus
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Abbas Bader indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Pawel Szurnicki indicated no relevant financial relationships.
Ifrah Fatima, MD1, Abbas Bader, 2, Noor Hassan, MD1, Mir Zulqarnain, DO1, Pawel Szurnicki, MD3. P3327 - “Snake-skin” Shedding Appearance of Mucosa in a Case of Esophagitis Dissecans Superficialis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
