Tuesday Poster Session
Category: Esophagus
P3328 - Novel Approaches to Manage Cervical Esophageal Perforation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- NB
Navtej Buttar, MD
Mayo Clinic
Rochester, Minnesota
Presenting Author(s)
Navtej S. Buttar, MD, Mayank Goyal, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Fnu Deepali, MBBS, Aya Akhras, MBBS, Shubham Sood, MBBS
Mayo Clinic, Rochester, MN
Introduction: Cervical esophageal perforation resulting from dilation poses unique challenges. If left untreated, it can lead to complications such as abscess formation, pleural effusion, and the development of esophagopleurocutaneous fistulas. Abscesses can also lead to esophagorespiratory fistulas. Managing these lesions is particularly challenging in patients with comorbidities who are poor surgical candidates. Placing a fully covered (FC) esophageal stent may not be possible due to limited landing space. Additionally, achieving a tight seal is difficult, and there is a risk of pressure necrosis and damage to the membranous trachea
Case Description/Methods: We describe a 72-year-old female who presented to the emergency department with severe chest pain. Upon evaluation, she was found to have an esophageal perforation with pneumomediastinum, which occurred as a complication of a dilation procedure performed eight hours earlier. Due to the patient's multiple comorbidities, including borderline cardiovascular status, deconditioning, gastrointestinal dysmotility, and recent pulmonary embolism, surgical intervention was not a suitable option.
Despite challenges of inserting esophageal stent like, proximal position causing foreign body sensation and difficulty to place sutures/clips, an attempt to put one was made that failed 2 days later. An EGD revealed a 5mm fistula found in the middle 3rd of the esophagus. Subsequently the stent was removed and a nasocystic drain was placed to drain the abscess cavity and turn the leak and the abscess into blind sinus tract. 5 days later the drain was removed and to manage the residual sinus tract, a double-J ureteral stent was considered. The rationale behind this was to prevent the re-accumulation of abscess and avoid trauma to the surrounding structures. An esophagogram revealed the leakage to be well controlled by the ureteral stent. Following the successful placement of ureteral stent, the patient was trialed on a clear liquid diet which she tolerated without difficulty and escalated to a full liquid diet. Further imaging revealed complete healing on the 15th day and the ureteral stent was removed
Discussion: We have successfully described a simple 2 step approach in the management of an esophageal fistula where an insertion of a standard FC esophageal stent was challenging. Here firstly a short-term trans nasal drain was used to eliminate the cavity and turn it into a blind sinus tract, secondly a ureteral stent was placed to manage the residual sinus tract

Disclosures:
Navtej S. Buttar, MD, Mayank Goyal, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Fnu Deepali, MBBS, Aya Akhras, MBBS, Shubham Sood, MBBS. P3328 - Novel Approaches to Manage Cervical Esophageal Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Cervical esophageal perforation resulting from dilation poses unique challenges. If left untreated, it can lead to complications such as abscess formation, pleural effusion, and the development of esophagopleurocutaneous fistulas. Abscesses can also lead to esophagorespiratory fistulas. Managing these lesions is particularly challenging in patients with comorbidities who are poor surgical candidates. Placing a fully covered (FC) esophageal stent may not be possible due to limited landing space. Additionally, achieving a tight seal is difficult, and there is a risk of pressure necrosis and damage to the membranous trachea
Case Description/Methods: We describe a 72-year-old female who presented to the emergency department with severe chest pain. Upon evaluation, she was found to have an esophageal perforation with pneumomediastinum, which occurred as a complication of a dilation procedure performed eight hours earlier. Due to the patient's multiple comorbidities, including borderline cardiovascular status, deconditioning, gastrointestinal dysmotility, and recent pulmonary embolism, surgical intervention was not a suitable option.
Despite challenges of inserting esophageal stent like, proximal position causing foreign body sensation and difficulty to place sutures/clips, an attempt to put one was made that failed 2 days later. An EGD revealed a 5mm fistula found in the middle 3rd of the esophagus. Subsequently the stent was removed and a nasocystic drain was placed to drain the abscess cavity and turn the leak and the abscess into blind sinus tract. 5 days later the drain was removed and to manage the residual sinus tract, a double-J ureteral stent was considered. The rationale behind this was to prevent the re-accumulation of abscess and avoid trauma to the surrounding structures. An esophagogram revealed the leakage to be well controlled by the ureteral stent. Following the successful placement of ureteral stent, the patient was trialed on a clear liquid diet which she tolerated without difficulty and escalated to a full liquid diet. Further imaging revealed complete healing on the 15th day and the ureteral stent was removed
Discussion: We have successfully described a simple 2 step approach in the management of an esophageal fistula where an insertion of a standard FC esophageal stent was challenging. Here firstly a short-term trans nasal drain was used to eliminate the cavity and turn it into a blind sinus tract, secondly a ureteral stent was placed to manage the residual sinus tract

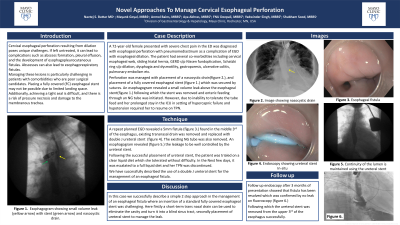
Figure: Image A showing esophageal stent and naso-cystic drain in white
Image B showing 5mm middle esophageal fistula
Image C showing placement of double J ureteral stent to close the leak
Image D shows esophagogram confirming no leak
Image B showing 5mm middle esophageal fistula
Image C showing placement of double J ureteral stent to close the leak
Image D shows esophagogram confirming no leak
Disclosures:
Navtej S. Buttar indicated no relevant financial relationships.
Mayank Goyal indicated no relevant financial relationships.
Anmol Bains indicated no relevant financial relationships.
Yadwinder Singh indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Aya Akhras indicated no relevant financial relationships.
Shubham Sood indicated no relevant financial relationships.
Navtej S. Buttar, MD, Mayank Goyal, MBBS, Anmol Bains, MBBS, Yadwinder Singh, MBBS, Fnu Deepali, MBBS, Aya Akhras, MBBS, Shubham Sood, MBBS. P3328 - Novel Approaches to Manage Cervical Esophageal Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
