Tuesday Poster Session
Category: Esophagus
P3331 - Pill Esophagitis as a Complication of Eosinophilic Esophagitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Melanie H. De Shadarevian, DO, MS
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Melanie H. De Shadarevian, DO, MS1, Quan M.. Nhu, MD, PhD2
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Clinic & Scripps Research Institute, La Jolla, CA
Introduction: Eosinophilic esophagitis (EoE) is a chronic, allergen-driven, immune-mediated disease of the esophagus that progresses to fibrostenotic EoE, resulting in esophageal dysfunction. Chronic untreated or inadequately controlled EoE causes symptoms related to esophageal dysmotility and dysfunction such as dysphagia and food impaction. Herein, we present a case of pill esophagitis in a healthy young male as a complication of untreated EoE.
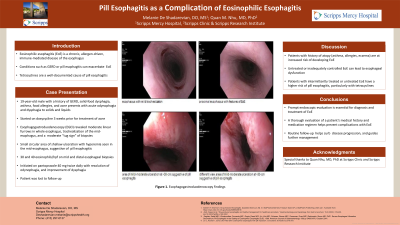
Case Description/Methods: A 19-year-old white male college student with a history of GERD not on therapy, chronic intermittent solid-food dysphagia for 6 years, asthma, food allergies, and acne presented with an acute onset of odynophagia. Odynophagia developed ten days prior and was described as a burning sensation of the throat with associated dysphagia to solids and liquids due to significant esophageal pain. He was started on doxycycline three weeks prior for treatment of acne. Doxycycline was discontinued at onset of odynophagia. Trial of over-the-counter omeprazole 20 mg daily over seven days provided minimal relief of odynophagia. Prompt esophagogastroduodenoscopy (EGD) revealed mild esophageal edema and pallor, moderate linear furrows throughout whole esophagus, and mild trachealization of the mid-esophagus. Esophageal biopsies exhibited a moderate “tug sign.” Careful inspection revealed a small circular area of mild-moderate shallow ulceration with hyperemia in the mid-esophagus, supporting doxycycline pill esophagitis. Distal and mid-esophageal biopsies showed 30 and 40 eosinophils/hpf, respectively, supporting a diagnosis of EoE. At the site of ulceration in the mid-esophagus, biopsies showed ulceration and granulation tissue, without foreign material, and were negative for CMV, HSV, or fungal organisms. Patient was treated empirically with viscous lidocaine 2% briefly for symptomatic relief and initiated on high-dose proton-pump inhibitor therapy twice daily for his new diagnosis of EoE. His odynophagia resolved on follow-up a few weeks later. Clinically, his dysphagia has improved on PPI therapy. Scheduling for follow-up EGD has not been successful.
Discussion: Esophageal dysfunction and dysmotility in chronic EoE contribute to food dysphagia and pill dysphagia, predisposing patients to pill esophagitis. Susceptible patients with dysphagia and EoE should be counseled appropriately when prescribed medications that are known to cause pill esophagitis. Our case emphasizes the need for prompt recognition and treatment of EoE to prevent future complications.
Disclosures:
Melanie H. De Shadarevian, DO, MS1, Quan M.. Nhu, MD, PhD2. P3331 - Pill Esophagitis as a Complication of Eosinophilic Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Clinic & Scripps Research Institute, La Jolla, CA
Introduction: Eosinophilic esophagitis (EoE) is a chronic, allergen-driven, immune-mediated disease of the esophagus that progresses to fibrostenotic EoE, resulting in esophageal dysfunction. Chronic untreated or inadequately controlled EoE causes symptoms related to esophageal dysmotility and dysfunction such as dysphagia and food impaction. Herein, we present a case of pill esophagitis in a healthy young male as a complication of untreated EoE.
Case Description/Methods: A 19-year-old white male college student with a history of GERD not on therapy, chronic intermittent solid-food dysphagia for 6 years, asthma, food allergies, and acne presented with an acute onset of odynophagia. Odynophagia developed ten days prior and was described as a burning sensation of the throat with associated dysphagia to solids and liquids due to significant esophageal pain. He was started on doxycycline three weeks prior for treatment of acne. Doxycycline was discontinued at onset of odynophagia. Trial of over-the-counter omeprazole 20 mg daily over seven days provided minimal relief of odynophagia. Prompt esophagogastroduodenoscopy (EGD) revealed mild esophageal edema and pallor, moderate linear furrows throughout whole esophagus, and mild trachealization of the mid-esophagus. Esophageal biopsies exhibited a moderate “tug sign.” Careful inspection revealed a small circular area of mild-moderate shallow ulceration with hyperemia in the mid-esophagus, supporting doxycycline pill esophagitis. Distal and mid-esophageal biopsies showed 30 and 40 eosinophils/hpf, respectively, supporting a diagnosis of EoE. At the site of ulceration in the mid-esophagus, biopsies showed ulceration and granulation tissue, without foreign material, and were negative for CMV, HSV, or fungal organisms. Patient was treated empirically with viscous lidocaine 2% briefly for symptomatic relief and initiated on high-dose proton-pump inhibitor therapy twice daily for his new diagnosis of EoE. His odynophagia resolved on follow-up a few weeks later. Clinically, his dysphagia has improved on PPI therapy. Scheduling for follow-up EGD has not been successful.
Discussion: Esophageal dysfunction and dysmotility in chronic EoE contribute to food dysphagia and pill dysphagia, predisposing patients to pill esophagitis. Susceptible patients with dysphagia and EoE should be counseled appropriately when prescribed medications that are known to cause pill esophagitis. Our case emphasizes the need for prompt recognition and treatment of EoE to prevent future complications.
Disclosures:
Melanie De Shadarevian indicated no relevant financial relationships.
Quan Nhu: Regeneron – Advisory Committee/Board Member, Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member.
Melanie H. De Shadarevian, DO, MS1, Quan M.. Nhu, MD, PhD2. P3331 - Pill Esophagitis as a Complication of Eosinophilic Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
