Tuesday Poster Session
Category: Esophagus
P3332 - Esophageal Granular Cell Tumor With Symptomatic Presentation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Marko Kozyk, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Marko Kozyk, MD1, Ivan Babii, MD2, Benjamin Secor, BS3, Kateryna Strubchevska, MD1
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2A. A. Shalimov National Institute of Surgery and Transplantology, Kyiv, Kyyiv, Ukraine; 3Oakland University William Beaumont, Royal Oak, MI
Introduction: Granular cell tumors make up 0.5% of all soft tissue tumors and were first thought to be muscular in origin, but now shown to have mostly neural cell origins from Schwannian derivation. They are most often benign lesions found in the skin, with other notable sites being tongue, respiratory tract, bladder, breast and gastrointestinal tract. Approximately 10 percent arise in the GI tract with the esophagus being the most common; however, it represents just 1% of benign esophageal tumors [1].
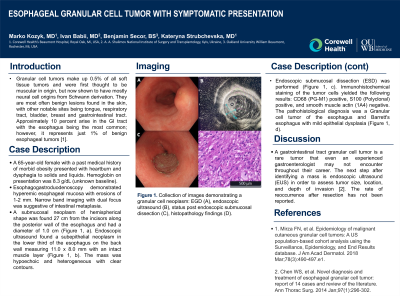
Case Description/Methods: A 65-year-old female with a past medical history of morbid obesity presented with heartburn and dysphagia to solids and liquids. Hemoglobin on presentation was 8.3 g/dL (unknown baseline). Esophagogastroduodenoscopy (EGD) demonstrated hyperemic esophageal mucousa with erosions of 1-2 mm. Narrow band imaging with dual focus was suggestive of intestinal metaplasia. A submucosal neoplasm of hemispherical shape was found 27 cm from the incisors along the posterior wall of the esophagus and had a diameter of 1.0 cm (Figure 1, a). Endoscopic ultrasound found a subepithelial neoplasm in the lower third of the esophagus on the back wall measuring 11.0 x 8.0 mm with an intact muscle layer (Figure 1, b). The mass was hypoechoic and heterogeneous with clear contours. Endoscopic submucosal dissection (ESD) was performed (Figure 1, c). Immunohistochemical staining of the tumor cells yielded the following results: CD68 (PG-M1) positive, S100 (Polyclonal) positive, and SmoothMuscleActin (1A4) negative. The pathohistological diagnosis was Granular cell tumor of the esophagus and Barrett's esophagus with mild epithelial dysplasia (Figure 1, d).
Discussion: A gastrointestinal tract granulosa cell tumor is a rare tumor that even an experienced gastroenterologist may not encounter throughout their career. The next step after identifying a mass is endoscopic ultrasound (EUS) in order to asses tumor size, location, and depth of invasion then resection for lesions over 1 cm [2]. The rate of reoccurrence after resection has not been reported.
References:
1. Mirza FN, et al. Epidemiology of malignant cutaneous granular cell tumors: A US population-based cohort analysis using the Surveillance, Epidemiology, and End Results database. J Am Acad Dermatol. 2018 Mar;78(3):490-497.e1.
2. Chen WS, et al. Novel diagnosis and treatment of esophageal granular cell tumor: report of 14 cases and review of the literature. Ann Thorac Surg. 2014 Jan;97(1):296-302.

Disclosures:
Marko Kozyk, MD1, Ivan Babii, MD2, Benjamin Secor, BS3, Kateryna Strubchevska, MD1. P3332 - Esophageal Granular Cell Tumor With Symptomatic Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2A. A. Shalimov National Institute of Surgery and Transplantology, Kyiv, Kyyiv, Ukraine; 3Oakland University William Beaumont, Royal Oak, MI
Introduction: Granular cell tumors make up 0.5% of all soft tissue tumors and were first thought to be muscular in origin, but now shown to have mostly neural cell origins from Schwannian derivation. They are most often benign lesions found in the skin, with other notable sites being tongue, respiratory tract, bladder, breast and gastrointestinal tract. Approximately 10 percent arise in the GI tract with the esophagus being the most common; however, it represents just 1% of benign esophageal tumors [1].
Case Description/Methods: A 65-year-old female with a past medical history of morbid obesity presented with heartburn and dysphagia to solids and liquids. Hemoglobin on presentation was 8.3 g/dL (unknown baseline). Esophagogastroduodenoscopy (EGD) demonstrated hyperemic esophageal mucousa with erosions of 1-2 mm. Narrow band imaging with dual focus was suggestive of intestinal metaplasia. A submucosal neoplasm of hemispherical shape was found 27 cm from the incisors along the posterior wall of the esophagus and had a diameter of 1.0 cm (Figure 1, a). Endoscopic ultrasound found a subepithelial neoplasm in the lower third of the esophagus on the back wall measuring 11.0 x 8.0 mm with an intact muscle layer (Figure 1, b). The mass was hypoechoic and heterogeneous with clear contours. Endoscopic submucosal dissection (ESD) was performed (Figure 1, c). Immunohistochemical staining of the tumor cells yielded the following results: CD68 (PG-M1) positive, S100 (Polyclonal) positive, and SmoothMuscleActin (1A4) negative. The pathohistological diagnosis was Granular cell tumor of the esophagus and Barrett's esophagus with mild epithelial dysplasia (Figure 1, d).
Discussion: A gastrointestinal tract granulosa cell tumor is a rare tumor that even an experienced gastroenterologist may not encounter throughout their career. The next step after identifying a mass is endoscopic ultrasound (EUS) in order to asses tumor size, location, and depth of invasion then resection for lesions over 1 cm [2]. The rate of reoccurrence after resection has not been reported.
References:
1. Mirza FN, et al. Epidemiology of malignant cutaneous granular cell tumors: A US population-based cohort analysis using the Surveillance, Epidemiology, and End Results database. J Am Acad Dermatol. 2018 Mar;78(3):490-497.e1.
2. Chen WS, et al. Novel diagnosis and treatment of esophageal granular cell tumor: report of 14 cases and review of the literature. Ann Thorac Surg. 2014 Jan;97(1):296-302.

Figure: Figure 1. Collection of images demonstrating a granular cell neoplasm: EGD (A), endoscopic ultrasound (B), status post endoscopic submucosal dissection (C), histopathology findings (D).
Disclosures:
Marko Kozyk indicated no relevant financial relationships.
Ivan Babii indicated no relevant financial relationships.
Benjamin Secor indicated no relevant financial relationships.
Kateryna Strubchevska indicated no relevant financial relationships.
Marko Kozyk, MD1, Ivan Babii, MD2, Benjamin Secor, BS3, Kateryna Strubchevska, MD1. P3332 - Esophageal Granular Cell Tumor With Symptomatic Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
