Tuesday Poster Session
Category: Esophagus
P3337 - Mucosal Blow Out: A Sequel of a Misdiagnosed Achalasia - A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ahmed H. abdelwahed, MBBCh
University of Connecticut-Hartford
Farmington, CT
Presenting Author(s)
Ahmed H. abdelwahed, MBBCh1, Amr Sayed, MD2, Ruchir paladiya, MD3, Mayra Sanchez, MD4, Amir Masoud, MD4
1University of Connecticut-Hartford, Farmington, CT; 2Norwalk Hospital, Norwalk, CT; 3University of Connecticut, Farmington, CT; 4Hartford Healthcare, Fairfield, CT
Introduction: Achalasia is a rare disorder that is characterized by impaired relaxation of the Lower esophageal sphincter and inadequate peristalsis. The Chicago classification aims to provide a standardized criteria for achalasia subtypes which has prognostic and management implications. We report a case that was misdiagnosed as achalasia and underwent Heller’s myotomy and eventually a per-oral endoscopic myotomy (POEM). Her case was complicated with esophageal mucosal blow out. The case highlights the devastating complications of acting upon inconclusive manometery data rather than the actual clinical picture.
Case Description/Methods: A 68 year-old lady with a history of GERD who presented with dysphagia to solid food and pills, heart burn and food regurgitation. She had an upper endoscopy that showed Schatzki's ring, hiatal hernia and reflux esophagitis. Her high resolution manometery showed diffuse esophageal spasm with low distal latency (less than 4.5 seconds) in 8 out of 10 swallows. Although the HRM demonstrated normal peristalsis, the high normal mean integrated relaxation pressure raised the concern for a developing achalasia type 3. She was referred for a Heller’s myotomy and DOR fundoplication. Her dysphagia improved initially but then worsened significantly. EndoFlip was initially concerning for a tight wrap and patient underwent balloon dilatation with some improvement. However, after an expert second opinion, her symptoms were attributed to a blown out myotomy (BOM) which was evident on the timed barium swallow. Decision was to proceed with Short segment POEM to correct the diverticulum. Patient’s symptoms improved slightly. However, she developed constipation. Her gastric emptying studies showed moderate gastroparesis which was attributed to iatrogenic vagal nerve injury. Unfortunately, she further had abrupt onset of severe dysphagia and EGD showed intussusception of the luminal of the stomach, which was surgically corrected with laparoscopic take down of the fundoplication.
Discussion: The patient's complex history, from initial presentation and misdiagnosis of achalasia to various interventions, highlights the difficulties and potential pitfalls in diagnosing and managing this condition. The absence of symptom relief despite multiple interventions indicates the need for comprehensive and cautious evaluation before proceeding with surgical interventions. Further studies like endo-Flip and timed barium swallow can be useful when HRM data is inconclusive.

Disclosures:
Ahmed H. abdelwahed, MBBCh1, Amr Sayed, MD2, Ruchir paladiya, MD3, Mayra Sanchez, MD4, Amir Masoud, MD4. P3337 - Mucosal Blow Out: A Sequel of a Misdiagnosed Achalasia - A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Connecticut-Hartford, Farmington, CT; 2Norwalk Hospital, Norwalk, CT; 3University of Connecticut, Farmington, CT; 4Hartford Healthcare, Fairfield, CT
Introduction: Achalasia is a rare disorder that is characterized by impaired relaxation of the Lower esophageal sphincter and inadequate peristalsis. The Chicago classification aims to provide a standardized criteria for achalasia subtypes which has prognostic and management implications. We report a case that was misdiagnosed as achalasia and underwent Heller’s myotomy and eventually a per-oral endoscopic myotomy (POEM). Her case was complicated with esophageal mucosal blow out. The case highlights the devastating complications of acting upon inconclusive manometery data rather than the actual clinical picture.
Case Description/Methods: A 68 year-old lady with a history of GERD who presented with dysphagia to solid food and pills, heart burn and food regurgitation. She had an upper endoscopy that showed Schatzki's ring, hiatal hernia and reflux esophagitis. Her high resolution manometery showed diffuse esophageal spasm with low distal latency (less than 4.5 seconds) in 8 out of 10 swallows. Although the HRM demonstrated normal peristalsis, the high normal mean integrated relaxation pressure raised the concern for a developing achalasia type 3. She was referred for a Heller’s myotomy and DOR fundoplication. Her dysphagia improved initially but then worsened significantly. EndoFlip was initially concerning for a tight wrap and patient underwent balloon dilatation with some improvement. However, after an expert second opinion, her symptoms were attributed to a blown out myotomy (BOM) which was evident on the timed barium swallow. Decision was to proceed with Short segment POEM to correct the diverticulum. Patient’s symptoms improved slightly. However, she developed constipation. Her gastric emptying studies showed moderate gastroparesis which was attributed to iatrogenic vagal nerve injury. Unfortunately, she further had abrupt onset of severe dysphagia and EGD showed intussusception of the luminal of the stomach, which was surgically corrected with laparoscopic take down of the fundoplication.
Discussion: The patient's complex history, from initial presentation and misdiagnosis of achalasia to various interventions, highlights the difficulties and potential pitfalls in diagnosing and managing this condition. The absence of symptom relief despite multiple interventions indicates the need for comprehensive and cautious evaluation before proceeding with surgical interventions. Further studies like endo-Flip and timed barium swallow can be useful when HRM data is inconclusive.

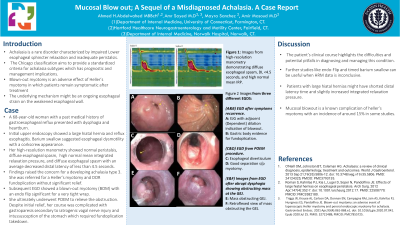
Figure: Figure (1) A, B, C, D Images from EGD done after symptoms recurrence suggesting BOM
E,F: Images from EGD after Abrupt Dysphagia showing obstructing mass at the GEJ
A: Food bolus in the lower third of the esophagus
B: Removal of food Bolus
C: EJG with Adjacent (Dependent) Dilation indication of Blow out
D: Gastric Body evidence for Fundoplication
E: Mass obstructing GEJ
F: Retroflexed View of mass obstructing the GEJ
E,F: Images from EGD after Abrupt Dysphagia showing obstructing mass at the GEJ
A: Food bolus in the lower third of the esophagus
B: Removal of food Bolus
C: EJG with Adjacent (Dependent) Dilation indication of Blow out
D: Gastric Body evidence for Fundoplication
E: Mass obstructing GEJ
F: Retroflexed View of mass obstructing the GEJ
Disclosures:
Ahmed abdelwahed indicated no relevant financial relationships.
Amr Sayed indicated no relevant financial relationships.
Ruchir paladiya indicated no relevant financial relationships.
Mayra Sanchez indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Ahmed H. abdelwahed, MBBCh1, Amr Sayed, MD2, Ruchir paladiya, MD3, Mayra Sanchez, MD4, Amir Masoud, MD4. P3337 - Mucosal Blow Out: A Sequel of a Misdiagnosed Achalasia - A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

