Tuesday Poster Session
Category: Esophagus
P3346 - Pemphigus Vulgaris: A Rare Cause of Esophagitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Navjit Singh, MD
University of Illinois College of Medicine at Peoria
Peoria, IL
Presenting Author(s)
Navjit Singh, MD, Lavneet Chawla, MD, Yeshaswini Panathur Sreenivasa, MD, Jason Bill, MD
University of Illinois College of Medicine at Peoria, Peoria, IL
Introduction: Pemphigus vulgaris (PV) is the most common, but a life-threatening subtype of pemphigus with a mortality rate of 5-15%. Esophageal PV is an underdiagnosed entity. The most common presenting symptoms in patients with esophageal PV are dysphagia and odynophagia, 57.1% and 21.4%, respectively. It takes several months to accurately diagnose PV and even longer to achieve treatment goals to improve clinical outcomes.
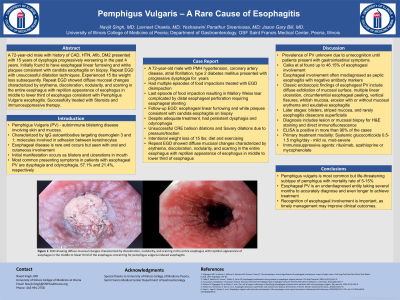
Case Description/Methods: A 72-year-old male with a history of hypertension, type 2 diabetes mellitus presented with a 15-year history of dysphagia. He had been lost to follow-up and now reported worsening dysphagia. He reported 15 lbs intentional weight loss in one year with diet and exercising. He denied any other symptoms including skin changes. He was found to have Candida esophagitis on esophagogastroduodenoscopy (EGD). Despite adequate treatment, he had persistent dysphagia and odynophagia. Serial esophageal dilatations were unsuccessful due to the pressure and traction. A barium swallow study showed a diffusely small caliber esophagus without any peristaltic abnormalities. Repeat EGD revealed diffuse mucosal changes characterized by erythema, discoloration, nodularity, and scarring in the entire esophagus with reptilian appearance in the middle to lower third of the esophagus, seen in figure 1. Biopsies confirmed PV esophagitis. Patient was started on prednisone therapy with a taper, and daily 100 mg azathioprine which he tolerated well.
Discussion: Pemphigus vulgaris with esophageal involvement is rare. The prevalence of esophageal involvement in PV is unknown due to delayed recognition. PV is caused by antibody mediated autoimmune reaction to epithelial cell surface antigens causing acantholysis. It is often misdiagnosed as peptic esophagitis as desmoglein antibody markers can be negative and patient rarely have classic PV skin findings. Classic EGD findings of esophageal PV include diffuse exfoliation of mucosal surface, multiple linear ulceration, circumferential esophageal peeling, vertical fissures, erosion with or without mucosal erythema and exudative esophagitis. In later stages, esophageal mucosal findings of PV may develop into blisters, striped mucosa, and rarely esophagitis dissecans superficialis. Systemic glucocorticoids are the primary treatment modality for PV. Immunosuppressive agents including rituximab, azathioprine or mycophenolate are given concurrently or after steroids for improved efficacy of immunosuppressive therapy.

Disclosures:
Navjit Singh, MD, Lavneet Chawla, MD, Yeshaswini Panathur Sreenivasa, MD, Jason Bill, MD. P3346 - Pemphigus Vulgaris: A Rare Cause of Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Illinois College of Medicine at Peoria, Peoria, IL
Introduction: Pemphigus vulgaris (PV) is the most common, but a life-threatening subtype of pemphigus with a mortality rate of 5-15%. Esophageal PV is an underdiagnosed entity. The most common presenting symptoms in patients with esophageal PV are dysphagia and odynophagia, 57.1% and 21.4%, respectively. It takes several months to accurately diagnose PV and even longer to achieve treatment goals to improve clinical outcomes.
Case Description/Methods: A 72-year-old male with a history of hypertension, type 2 diabetes mellitus presented with a 15-year history of dysphagia. He had been lost to follow-up and now reported worsening dysphagia. He reported 15 lbs intentional weight loss in one year with diet and exercising. He denied any other symptoms including skin changes. He was found to have Candida esophagitis on esophagogastroduodenoscopy (EGD). Despite adequate treatment, he had persistent dysphagia and odynophagia. Serial esophageal dilatations were unsuccessful due to the pressure and traction. A barium swallow study showed a diffusely small caliber esophagus without any peristaltic abnormalities. Repeat EGD revealed diffuse mucosal changes characterized by erythema, discoloration, nodularity, and scarring in the entire esophagus with reptilian appearance in the middle to lower third of the esophagus, seen in figure 1. Biopsies confirmed PV esophagitis. Patient was started on prednisone therapy with a taper, and daily 100 mg azathioprine which he tolerated well.
Discussion: Pemphigus vulgaris with esophageal involvement is rare. The prevalence of esophageal involvement in PV is unknown due to delayed recognition. PV is caused by antibody mediated autoimmune reaction to epithelial cell surface antigens causing acantholysis. It is often misdiagnosed as peptic esophagitis as desmoglein antibody markers can be negative and patient rarely have classic PV skin findings. Classic EGD findings of esophageal PV include diffuse exfoliation of mucosal surface, multiple linear ulceration, circumferential esophageal peeling, vertical fissures, erosion with or without mucosal erythema and exudative esophagitis. In later stages, esophageal mucosal findings of PV may develop into blisters, striped mucosa, and rarely esophagitis dissecans superficialis. Systemic glucocorticoids are the primary treatment modality for PV. Immunosuppressive agents including rituximab, azathioprine or mycophenolate are given concurrently or after steroids for improved efficacy of immunosuppressive therapy.

Figure: Figure 1: EGD showing diffuse mucosal changes characterized by discoloration, nodularity, and scarring in the entire esophagus with reptilian appearance of esophagus in the middle to lower third of the esophagus consistent with pemphigus vulgaris esophagitis.
Disclosures:
Navjit Singh indicated no relevant financial relationships.
Lavneet Chawla indicated no relevant financial relationships.
Yeshaswini Panathur Sreenivasa indicated no relevant financial relationships.
Jason Bill indicated no relevant financial relationships.
Navjit Singh, MD, Lavneet Chawla, MD, Yeshaswini Panathur Sreenivasa, MD, Jason Bill, MD. P3346 - Pemphigus Vulgaris: A Rare Cause of Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
