Tuesday Poster Session
Category: Esophagus
P3355 - Esophagitis Dissecans Superficialis Presenting as a Rare Cause of Dysphagia in a Patient With Chronic Ibuprofen Use
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Hannah W. Fiske, MD
Brown University/Rhode Island Hospital
Providence, RI
Presenting Author(s)
Hannah W. Fiske, MD1, Breton Roussel, MD2, Jim ChunHao. Lee, MD, MPH3, Ronan Farrell, MD4
1Brown University/Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Rhode Island Hospital, Providence, RI; 4Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: The differential for esophageal dysphagia is broad and includes anatomic obstruction from stricture or malignancy, motility disorders, and inflammatory conditions such as eosinophilic esophagitis. The approach to the diagnostic evaluation of dysphagia is largely based on patient history, but often requires endoscopic evaluation. Outcomes and treatment plans vary widely based on eventual diagnosis, so the process of determining the underlying cause of dysphagia is critical and time sensitive.
Case Description/Methods: An 88-year-old female with no significant past medical history presented to the ED with lower back pain and lower extremity weakness in the setting of a known T10 compression/burst fracture. She had been managing her pain with significant amounts of ibuprofen. She was diagnosed with spinal stenosis with thoracic myelopathy, and underwent successful orthopedic treatment with no subsequent complications. During her admission she also endorsed 3 months of progressive dysphagia, globus sensation in her upper chest with oral intake, and an accompanying five pound weight loss. She denied nausea, vomiting, odynophagia, abdominal pain, early satiety, or fevers. She had no family history of esophageal malignancy, denied tobacco use, and endorsed minimal alcohol intake. She had never undergone endoscopy (EGD). Oropharyngeal exam was normal. The severity of her symptoms ultimately presented a barrier to discharge. An inpatient EGD demonstrated severe esophagitis with linear white desquamating fragments of peeling esophageal epithelium, consistent with esophagitis dissecans superficialis (EDS). Biopsies were obtained. Patient was started on twice daily omeprazole, counseled on avoidance of NSAIDs, and scheduled for repeat EGD in 8 weeks.
Discussion: EDS is a rare benign pathology of the esophagus characterized on EGD with long, vertical, superficial white strips of peeling esophageal epithelium with a normal underlying mucosal layer. Given its rarity, the pathogenesis of EDS is largely unknown. However, cases of EDS have been associated with trauma, motility disorders, immunosuppression, toxins, including smoking and alcohol, and medications, including NSAIDs, bisphosphonates, and anti-depressants. In the case described here, the most likely trigger was chronic NSAID use resulting in mucosal injury. Though it has dramatic esophageal findings, reassuringly this benign condition most often completely resolves with withdrawal of the causative agent.

Disclosures:
Hannah W. Fiske, MD1, Breton Roussel, MD2, Jim ChunHao. Lee, MD, MPH3, Ronan Farrell, MD4. P3355 - Esophagitis Dissecans Superficialis Presenting as a Rare Cause of Dysphagia in a Patient With Chronic Ibuprofen Use, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brown University/Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Rhode Island Hospital, Providence, RI; 4Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: The differential for esophageal dysphagia is broad and includes anatomic obstruction from stricture or malignancy, motility disorders, and inflammatory conditions such as eosinophilic esophagitis. The approach to the diagnostic evaluation of dysphagia is largely based on patient history, but often requires endoscopic evaluation. Outcomes and treatment plans vary widely based on eventual diagnosis, so the process of determining the underlying cause of dysphagia is critical and time sensitive.
Case Description/Methods: An 88-year-old female with no significant past medical history presented to the ED with lower back pain and lower extremity weakness in the setting of a known T10 compression/burst fracture. She had been managing her pain with significant amounts of ibuprofen. She was diagnosed with spinal stenosis with thoracic myelopathy, and underwent successful orthopedic treatment with no subsequent complications. During her admission she also endorsed 3 months of progressive dysphagia, globus sensation in her upper chest with oral intake, and an accompanying five pound weight loss. She denied nausea, vomiting, odynophagia, abdominal pain, early satiety, or fevers. She had no family history of esophageal malignancy, denied tobacco use, and endorsed minimal alcohol intake. She had never undergone endoscopy (EGD). Oropharyngeal exam was normal. The severity of her symptoms ultimately presented a barrier to discharge. An inpatient EGD demonstrated severe esophagitis with linear white desquamating fragments of peeling esophageal epithelium, consistent with esophagitis dissecans superficialis (EDS). Biopsies were obtained. Patient was started on twice daily omeprazole, counseled on avoidance of NSAIDs, and scheduled for repeat EGD in 8 weeks.
Discussion: EDS is a rare benign pathology of the esophagus characterized on EGD with long, vertical, superficial white strips of peeling esophageal epithelium with a normal underlying mucosal layer. Given its rarity, the pathogenesis of EDS is largely unknown. However, cases of EDS have been associated with trauma, motility disorders, immunosuppression, toxins, including smoking and alcohol, and medications, including NSAIDs, bisphosphonates, and anti-depressants. In the case described here, the most likely trigger was chronic NSAID use resulting in mucosal injury. Though it has dramatic esophageal findings, reassuringly this benign condition most often completely resolves with withdrawal of the causative agent.

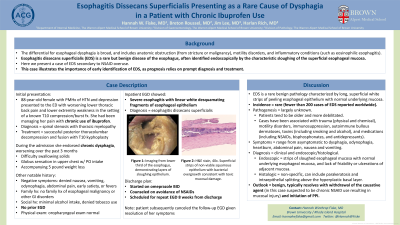
Figure: Figure 1:
(a) Endoscopic image showing mucosal sloughing of the lower third of the esophagus.
(b-c) H&E stain, magnification 20x (b) and 40x (c), showing superficial strips of non-viable squamous epithelium with bacterial overgrowth consistent with toxic mucosal damage; images reveal splitting of the superficial squamous epithelium and bacterial overgrowth in between layers.
(a) Endoscopic image showing mucosal sloughing of the lower third of the esophagus.
(b-c) H&E stain, magnification 20x (b) and 40x (c), showing superficial strips of non-viable squamous epithelium with bacterial overgrowth consistent with toxic mucosal damage; images reveal splitting of the superficial squamous epithelium and bacterial overgrowth in between layers.
Disclosures:
Hannah Fiske indicated no relevant financial relationships.
Breton Roussel indicated no relevant financial relationships.
Jim Lee indicated no relevant financial relationships.
Ronan Farrell indicated no relevant financial relationships.
Hannah W. Fiske, MD1, Breton Roussel, MD2, Jim ChunHao. Lee, MD, MPH3, Ronan Farrell, MD4. P3355 - Esophagitis Dissecans Superficialis Presenting as a Rare Cause of Dysphagia in a Patient With Chronic Ibuprofen Use, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
