Tuesday Poster Session
Category: Functional Bowel Disease
P3360 - Cromolyn Reduces Symptoms in Patients With Irritable Bowel Syndrome, Functional Dyspepsia, or Gastroparesis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Elisa Karhu, MD, MS
Stanford University
Stanford, CA
Presenting Author(s)
Elisa Karhu, MD, MS1, Linda Anh Nguyen, MD2, Irene Sonu, MD3, Leila Neshatian, MD, MSc4, Andres Gottfried-Blackmore, MD, PhD1, Nielsen Fernandez-Becker, MD, PhD2, Sean Spencer, MD, PhD5
1Stanford University, Stanford, CA; 2Stanford University, Redwood City, CA; 3Stanford University School of Medicine, Redwood City, CA; 4Stanford, Redwood City, CA; 5Stanford University, Palo Alto, CA
Introduction: Mucosal immune dysregulation characterized by mucosal mast cells and eosinophils has been described in patients with irritable bowel syndrome (IBS), functional dyspepsia (FD) and gastroparesis (GP). Additionally, patients with atopy are more likely to be diagnosed with IBS or FD. We hypothesize that cromolyn, a mast cell stabilizer, reduces symptoms in patients with IBS, FD and GP.
Methods: Retrospective analysis of patients with IBS, FD or GP treated with oral cromolyn sodium between 2015-2022. Comorbid conditions associated with immune dysregulation [Ehlers-Danlos syndrome (EDS), postural orthostatic tachycardia (POTS), mast cell activation disorder (MCAS) and atopy] were included to determine factors associated with response to therapy, as defined by patient-reported global improvement of symptoms. Statistical analyses were performed using Fisher’s exact test to determine response rates by diagnosis. Multiple logistic regression analysis was used to determine association between underlying comorbidities.
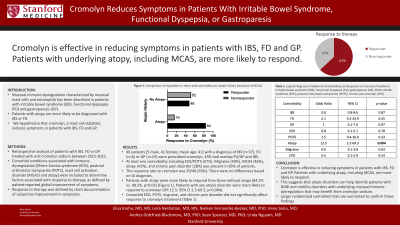
Results: 46 patients [5 male, 41 female; mean age: 41] with a diagnosis of IBS (n=37), FD (n=6) or GP (n=25) were prescribed cromolyn. 43% had overlap FD/GP and IBS. At least one comorbidity including EDS/POTS (57%), Migraine (50%), MCAS (46%), atopy (41%), and chronic pain disorder (28%) was present in 85% of patients. The response rate to cromolyn was 29/46 (63%). There were no differences based on GI diagnosis. Patients with atopy were more likely to respond than those without atopy (84.2% vs. 48.2%, p=0.02) (Figure 1). Patients with any atopic disorder were more likely to respond to cromolyn (OR 12.5; 95% CI 2.3-69.3, p=0.004). Comorbid EDS, POTS, migraine, and chronic pain disorder did not significantly affect response to cromolyn treatment (Table 1). Perceived lack of efficacy of cromolyn sodium was the most common reason for discontinuation. GI side effects accounted for discontinuation in 22% of patients. Perceived lack of efficacy of cromolyn sodium was the most common reason for discontinuation. GI side effects accounted for discontinuation in 22% of patients.
Discussion: Cromolyn is effective in reducing symptoms in patients with IBS, FD and GP. Patients with underlying atopy, including MCAS, are more likely to respond. This suggests that atopic disorders can help identify patients with DGBI and motility disorders with underlying mucosal immune dysregulation that may benefit from cromolyn sodium. Larger randomized controlled trials are warranted to confirm these findings.

Disclosures:
Elisa Karhu, MD, MS1, Linda Anh Nguyen, MD2, Irene Sonu, MD3, Leila Neshatian, MD, MSc4, Andres Gottfried-Blackmore, MD, PhD1, Nielsen Fernandez-Becker, MD, PhD2, Sean Spencer, MD, PhD5. P3360 - Cromolyn Reduces Symptoms in Patients With Irritable Bowel Syndrome, Functional Dyspepsia, or Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford University, Stanford, CA; 2Stanford University, Redwood City, CA; 3Stanford University School of Medicine, Redwood City, CA; 4Stanford, Redwood City, CA; 5Stanford University, Palo Alto, CA
Introduction: Mucosal immune dysregulation characterized by mucosal mast cells and eosinophils has been described in patients with irritable bowel syndrome (IBS), functional dyspepsia (FD) and gastroparesis (GP). Additionally, patients with atopy are more likely to be diagnosed with IBS or FD. We hypothesize that cromolyn, a mast cell stabilizer, reduces symptoms in patients with IBS, FD and GP.
Methods: Retrospective analysis of patients with IBS, FD or GP treated with oral cromolyn sodium between 2015-2022. Comorbid conditions associated with immune dysregulation [Ehlers-Danlos syndrome (EDS), postural orthostatic tachycardia (POTS), mast cell activation disorder (MCAS) and atopy] were included to determine factors associated with response to therapy, as defined by patient-reported global improvement of symptoms. Statistical analyses were performed using Fisher’s exact test to determine response rates by diagnosis. Multiple logistic regression analysis was used to determine association between underlying comorbidities.
Results: 46 patients [5 male, 41 female; mean age: 41] with a diagnosis of IBS (n=37), FD (n=6) or GP (n=25) were prescribed cromolyn. 43% had overlap FD/GP and IBS. At least one comorbidity including EDS/POTS (57%), Migraine (50%), MCAS (46%), atopy (41%), and chronic pain disorder (28%) was present in 85% of patients. The response rate to cromolyn was 29/46 (63%). There were no differences based on GI diagnosis. Patients with atopy were more likely to respond than those without atopy (84.2% vs. 48.2%, p=0.02) (Figure 1). Patients with any atopic disorder were more likely to respond to cromolyn (OR 12.5; 95% CI 2.3-69.3, p=0.004). Comorbid EDS, POTS, migraine, and chronic pain disorder did not significantly affect response to cromolyn treatment (Table 1). Perceived lack of efficacy of cromolyn sodium was the most common reason for discontinuation. GI side effects accounted for discontinuation in 22% of patients. Perceived lack of efficacy of cromolyn sodium was the most common reason for discontinuation. GI side effects accounted for discontinuation in 22% of patients.
Discussion: Cromolyn is effective in reducing symptoms in patients with IBS, FD and GP. Patients with underlying atopy, including MCAS, are more likely to respond. This suggests that atopic disorders can help identify patients with DGBI and motility disorders with underlying mucosal immune dysregulation that may benefit from cromolyn sodium. Larger randomized controlled trials are warranted to confirm these findings.

Figure: Figure 1: Comparison of responders in those with and without an atopic history (exclusive of MCAS).
Disclosures:
Elisa Karhu indicated no relevant financial relationships.
Linda Anh Nguyen: Ardelyx – Consultant. Atmo Biosciences – Consultant. Bold Health – Grant/Research Support. Evoke – Consultant. Gemelli – Consultant. Impel – Consultant. Neurogastryx – Consultant. Pendulum – Consultant. Phathom – Consultant. RosVivo – Advisor or Review Panel Member. Takeda – Consultant.
Irene Sonu: Bold Health – Grant/Research Support.
Leila Neshatian: salix, Ardelyx, GI supply, Vibrant – Advisory Committee/Board Member, Consultant.
Andres Gottfried-Blackmore indicated no relevant financial relationships.
Nielsen Fernandez-Becker indicated no relevant financial relationships.
Sean Spencer indicated no relevant financial relationships.
Elisa Karhu, MD, MS1, Linda Anh Nguyen, MD2, Irene Sonu, MD3, Leila Neshatian, MD, MSc4, Andres Gottfried-Blackmore, MD, PhD1, Nielsen Fernandez-Becker, MD, PhD2, Sean Spencer, MD, PhD5. P3360 - Cromolyn Reduces Symptoms in Patients With Irritable Bowel Syndrome, Functional Dyspepsia, or Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
