Tuesday Poster Session
Category: Functional Bowel Disease
P3366 - Where Is the DRE? Digital Rectal Exams are Infrequently Performed Prior to Anorectal Manometry
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Joseph A. Menand, MD
Mount Sinai Morningside-West
New York, NY
Presenting Author(s)
Joseph A. Menand, MD1, Robinderpal Sandhu, MD1, Ahmun Zafar, DO1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Michael S.. Smith, MD, MBA2, Jean Saleh, MD3, Daniela Jodorkovsky, MD4, Yuying Luo, MD5
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Mount Sinai, New York, NY; 5Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Dyssynergic defecation (DD) is a common cause of constipation in patients not responding to pharmacologic therapy. A diagnostic digital rectal examination (DRE) should be performed prior to referral for anorectal manometry (ARM) as studies have shown that DRE has similar sensitivity and specificity in diagnosing DD when performed by a skilled provider. It is unclear how frequently DRE is performed prior to ARM, and whether DRE findings can predict a diagnosis of DD on ARM in a real-world setting with a range of providers.
Methods: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics were compared using Chi-squared and Fischer’s Exact Tests. Our primary outcome was the proportion of patients who had a DRE prior to ARM; secondary outcomes included the concordance between DRE findings and diagnosis of DD.
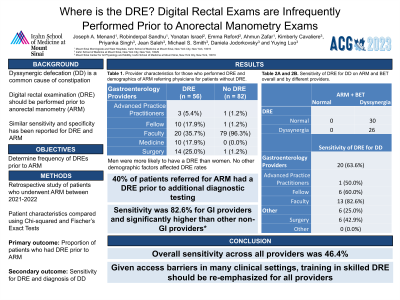
Results: Our study included 166 patients, with 67 (40.3%) having a documented DRE prior to ARM (Table 1). There were no significant differences in age, gender, race, BMI and English as primary language between patients who did and did not receive a DRE. The majority (58.2%) of DREs were performed by gastroenterology providers (attendings, fellows or nurse practitioners). Patients with a DRE were more likely to have a dyssynergic pattern on ARM (p = .030); however, there were no significant differences in the proportion of patients with rectal hyper- or hyposensitivity, present recto-anal inhibitory reflex, or abnormal balloon expulsion test. Of the DREs performed by gastroenterology providers, 57.9% had findings concordant with ARM results, which was significantly higher than for DREs by non-GI providers (30.8%, p = .007).
Discussion: In our study, only 40% of patients referred for ARM had a DRE prior to additional diagnostic testing. The majority of DREs were administered by gastroenterology providers, yet these examinations were only 57.9% concordant with ARM findings. While concordance was lower than previously reported, it was significantly higher than non-GI providers. Given access barriers to ARM in many clinical settings, as well as previous reports of high concordance between DRE and ARM, training in a skilled DRE should be re-emphasized for all levels of clinical providers.
Disclosures:
Joseph A. Menand, MD1, Robinderpal Sandhu, MD1, Ahmun Zafar, DO1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Michael S.. Smith, MD, MBA2, Jean Saleh, MD3, Daniela Jodorkovsky, MD4, Yuying Luo, MD5. P3366 - Where Is the DRE? Digital Rectal Exams are Infrequently Performed Prior to Anorectal Manometry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Morningside-West, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY; 4Mount Sinai, New York, NY; 5Center of GI Physiology and Motility at Mount Sinai West, New York, NY
Introduction: Dyssynergic defecation (DD) is a common cause of constipation in patients not responding to pharmacologic therapy. A diagnostic digital rectal examination (DRE) should be performed prior to referral for anorectal manometry (ARM) as studies have shown that DRE has similar sensitivity and specificity in diagnosing DD when performed by a skilled provider. It is unclear how frequently DRE is performed prior to ARM, and whether DRE findings can predict a diagnosis of DD on ARM in a real-world setting with a range of providers.
Methods: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics were compared using Chi-squared and Fischer’s Exact Tests. Our primary outcome was the proportion of patients who had a DRE prior to ARM; secondary outcomes included the concordance between DRE findings and diagnosis of DD.
Results: Our study included 166 patients, with 67 (40.3%) having a documented DRE prior to ARM (Table 1). There were no significant differences in age, gender, race, BMI and English as primary language between patients who did and did not receive a DRE. The majority (58.2%) of DREs were performed by gastroenterology providers (attendings, fellows or nurse practitioners). Patients with a DRE were more likely to have a dyssynergic pattern on ARM (p = .030); however, there were no significant differences in the proportion of patients with rectal hyper- or hyposensitivity, present recto-anal inhibitory reflex, or abnormal balloon expulsion test. Of the DREs performed by gastroenterology providers, 57.9% had findings concordant with ARM results, which was significantly higher than for DREs by non-GI providers (30.8%, p = .007).
Discussion: In our study, only 40% of patients referred for ARM had a DRE prior to additional diagnostic testing. The majority of DREs were administered by gastroenterology providers, yet these examinations were only 57.9% concordant with ARM findings. While concordance was lower than previously reported, it was significantly higher than non-GI providers. Given access barriers to ARM in many clinical settings, as well as previous reports of high concordance between DRE and ARM, training in a skilled DRE should be re-emphasized for all levels of clinical providers.
Disclosures:
Joseph Menand indicated no relevant financial relationships.
Robinderpal Sandhu indicated no relevant financial relationships.
Ahmun Zafar indicated no relevant financial relationships.
Yonatan Israel indicated no relevant financial relationships.
Emma Reford indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Priyanka Singh indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Medical – Consultant. Steris Endoscopy – Consultant.
Jean Saleh indicated no relevant financial relationships.
Daniela Jodorkovsky: ATMO Biosciences – Consultant.
Yuying Luo indicated no relevant financial relationships.
Joseph A. Menand, MD1, Robinderpal Sandhu, MD1, Ahmun Zafar, DO1, Yonatan Israel, BS2, Emma Reford, BA2, Kimberly Cavaliere, MD1, Priyanka Singh, MD1, Michael S.. Smith, MD, MBA2, Jean Saleh, MD3, Daniela Jodorkovsky, MD4, Yuying Luo, MD5. P3366 - Where Is the DRE? Digital Rectal Exams are Infrequently Performed Prior to Anorectal Manometry, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
