Tuesday Poster Session
Category: Functional Bowel Disease
P3368 - Gender and Differences in Diagnosis and Management of Veterans With IBS: A Retrospective Cohort Study Within a VA Health Care System
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Pierce L. Claassen, BS
Washington State University, Elson S. Floyd College of Medicine
Spokane, WA
Presenting Author(s)
Pierce L. Claassen, BS1, Jordyn N. Becker, BS2, Celeste K. L.. Cravalho, BS2, Garett Cecchini, BS2, Paulene Cay, BS2, Amneet Rai, PharmD3, Mark S. Riddle, MD, DrPH3
1Washington State University, Elson S. Floyd College of Medicine, Spokane, WA; 2University of Nevada, Reno School of Medicine, Reno, NV; 3VA Sierra Nevada Health Care System, Reno, NV
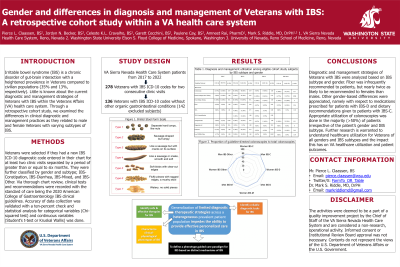
Introduction: Irritable bowel syndrome (IBS) is a chronic disorder of gut-brain interaction with a heightened prevalence in Veterans (35%), compared to the general population (13%). Little is known about the current diagnostic and management strategies of Veterans with IBS within the Veteran Affairs (VA) health care system. Through a retrospective cohort study, we examined the relationship between clinical practices and Veteran gender and IBS subtype at a VA medical center.
Methods: Veterans were selected if they had a new IBS diagnostic code entered in their chart for at least two clinic visits separated by a period of ≥ six months. They were further classified by gender and subtype; IBS-C, IBS-D, IBS-M, and IBS-Other. Via chart review, testing and recommendations were recorded with the standard of care being the American College of Gastroenterology IBS clinical guidelines. Accuracy was validated with a ten-percent check and statistical analysis for categorical variables (Chi-squared test) and continuous variables (Student’s T-test or Kruskal Wallis) was done.
Results: Chart review of 136 eligible Veterans (32 female) with IBS was done. Subtype breakdown was IBS-C (14), IBS-D (60), IBS-M (22), and IBS-O (40). Avoiding antispasmodics was observed more often in females than males (84.4% vs. 67.3%, p=0.075). Providers were less likely to recommend probiotics for IBS-C compared to IBS-D, IBS-M, and IBS-O (21.4% vs 50.0%, 50.0%, 52.5%, respectively) and less likely for females than males (37.5% vs. 51.0%, p=0.266). The likelihood of recommending fiber was relatively similar for IBS-C, IBS-D, IBS-M, and IBS-O (42.9%, 46.7%, 54.5% and 45.0%, respectively). Fiber was recommended to females and males at essentially equal rates (46.9% vs. 47.1%, p=1.00). A low FODMAP diet was more likely to be utilized in patients with IBS-D and IBS-M (20.0% and 18.2%) than with IBS-C and IBS-O (7.1% and 7.5%), and more likely to be recommended to females than males (21.9% vs. 12.5%, p=0.190).
Discussion: Diagnostic and management strategies of Veterans with IBS were analyzed based on IBS subtype and gender. Fiber was not recommended in the majority of patients, but nearly twice as likely to be recommended to females than males. Other gender-based differences were appreciated, namely with respect to medications for IBS-D and dietary recommendations for IBS-C. Further research is warranted to understand healthcare utilization for Veterans of all genders and IBS subtypes.
Disclosures:
Pierce L. Claassen, BS1, Jordyn N. Becker, BS2, Celeste K. L.. Cravalho, BS2, Garett Cecchini, BS2, Paulene Cay, BS2, Amneet Rai, PharmD3, Mark S. Riddle, MD, DrPH3. P3368 - Gender and Differences in Diagnosis and Management of Veterans With IBS: A Retrospective Cohort Study Within a VA Health Care System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Washington State University, Elson S. Floyd College of Medicine, Spokane, WA; 2University of Nevada, Reno School of Medicine, Reno, NV; 3VA Sierra Nevada Health Care System, Reno, NV
Introduction: Irritable bowel syndrome (IBS) is a chronic disorder of gut-brain interaction with a heightened prevalence in Veterans (35%), compared to the general population (13%). Little is known about the current diagnostic and management strategies of Veterans with IBS within the Veteran Affairs (VA) health care system. Through a retrospective cohort study, we examined the relationship between clinical practices and Veteran gender and IBS subtype at a VA medical center.
Methods: Veterans were selected if they had a new IBS diagnostic code entered in their chart for at least two clinic visits separated by a period of ≥ six months. They were further classified by gender and subtype; IBS-C, IBS-D, IBS-M, and IBS-Other. Via chart review, testing and recommendations were recorded with the standard of care being the American College of Gastroenterology IBS clinical guidelines. Accuracy was validated with a ten-percent check and statistical analysis for categorical variables (Chi-squared test) and continuous variables (Student’s T-test or Kruskal Wallis) was done.
Results: Chart review of 136 eligible Veterans (32 female) with IBS was done. Subtype breakdown was IBS-C (14), IBS-D (60), IBS-M (22), and IBS-O (40). Avoiding antispasmodics was observed more often in females than males (84.4% vs. 67.3%, p=0.075). Providers were less likely to recommend probiotics for IBS-C compared to IBS-D, IBS-M, and IBS-O (21.4% vs 50.0%, 50.0%, 52.5%, respectively) and less likely for females than males (37.5% vs. 51.0%, p=0.266). The likelihood of recommending fiber was relatively similar for IBS-C, IBS-D, IBS-M, and IBS-O (42.9%, 46.7%, 54.5% and 45.0%, respectively). Fiber was recommended to females and males at essentially equal rates (46.9% vs. 47.1%, p=1.00). A low FODMAP diet was more likely to be utilized in patients with IBS-D and IBS-M (20.0% and 18.2%) than with IBS-C and IBS-O (7.1% and 7.5%), and more likely to be recommended to females than males (21.9% vs. 12.5%, p=0.190).
Discussion: Diagnostic and management strategies of Veterans with IBS were analyzed based on IBS subtype and gender. Fiber was not recommended in the majority of patients, but nearly twice as likely to be recommended to females than males. Other gender-based differences were appreciated, namely with respect to medications for IBS-D and dietary recommendations for IBS-C. Further research is warranted to understand healthcare utilization for Veterans of all genders and IBS subtypes.
Disclosures:
Pierce Claassen indicated no relevant financial relationships.
Jordyn Becker indicated no relevant financial relationships.
Celeste Cravalho indicated no relevant financial relationships.
Garett Cecchini indicated no relevant financial relationships.
Paulene Cay indicated no relevant financial relationships.
Amneet Rai indicated no relevant financial relationships.
Mark Riddle: Pfizer, Inc. – Employee.
Pierce L. Claassen, BS1, Jordyn N. Becker, BS2, Celeste K. L.. Cravalho, BS2, Garett Cecchini, BS2, Paulene Cay, BS2, Amneet Rai, PharmD3, Mark S. Riddle, MD, DrPH3. P3368 - Gender and Differences in Diagnosis and Management of Veterans With IBS: A Retrospective Cohort Study Within a VA Health Care System, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
