Tuesday Poster Session
Category: Functional Bowel Disease
P3369 - Trends of Functional Dyspepsia Hospitalizations and Prevalence of Psychiatric and Non-Psychiatric Co-Morbidities: A Decade-Long Nationwide Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- VB
Vaishnavi Boppana, MD
University of New Mexico
Albuquerque, New Mexico
Presenting Author(s)
Rahul Pamarthy, MD1, Vaishnavi Boppana, MD2, Hassam Ali, MD3, Christopher Chang, MD, PhD4
1East Carolina University, Greenville, NC; 2University of New Mexico, Albuquerque, NM; 3ECU Health Medical Center / Brody School of Medicine, Greenville, NC; 4University of New Mexico Health Sciences Center, Albuquerque, NM
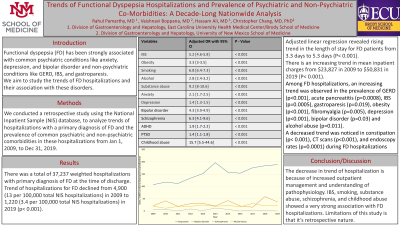
Introduction: Functional dyspepsia (FD) has been strongly associated with common psychiatric conditions like anxiety, depression, and bipolar disorder and non-psychiatric conditions like GERD, IBS, and gastroparesis. We aim to study the trends of FD hospitalizations and their association with these disorders.
Methods: We conducted a retrospective study using the National Inpatient Sample (NIS) database, to analyze trends of hospitalizations with a primary diagnosis of FD and the prevalence of common psychiatric and non-psychiatric comorbidities in these hospitalizations from Jan 1, 2009, to Dec 31, 2019.
Results: There was a total of 37,237 weighted hospitalizations with a primary diagnosis of FD at the time of discharge. The trend of hospitalizations for FD declined from 4,900 (13 per 100,000 total NIS hospitalizations) in 2009 to 1,220 (3.4 per 100,000 total NIS hospitalizations) in 2019 (p< 0.001). Adjusted linear regression revealed a rising trend in the length of stay for FD patients from 3.3 days in 2009 to 5.3 days in 2019 (P< 0.001); and an increasing trend in mean inpatient charges from $23,827 in 2009 to $50,831 in 2019 (P< 0.001). Among FD hospitalizations, an increasing trend was observed in the prevalence of PUD history (p=0.049), GERD (p< 0.001), acute pancreatitis (p=0.0008), IBS (p=0.0005), gastroparesis (p=0.019), obesity (p< 0.001), depression (p< 0.001), bipolar disorder (p=0.03) and alcohol abuse (p=0.011). A decreased trend was noticed in constipation (p< 0.001) during FD hospitalizations. On adjusted regression analysis, FD was strongly associated with history of PUD (2.8[2.5-3.2], p< 0.001), acute pancreatitis (3.3[3-3.8], p< 0.001), IBS (5.2[4.6-5.8], p< 0.001), gastroparesis (1.6[1.5-1.7], p< 0.001), obesity (3.3[3-3.5], p< 0.001), smoking (6.8[6.4-7.3], p< 0.001), alcohol (2.8[2.4-3.2], p< 0.001), substance abuse (9.2[8-10.6], p< 0.001), anxiety (2.1[1.7-2.5], p< 0.001), depression (1.4[1.3-1.5], p< 0.001), bipolar disorder (4.3[3.9-4.9], p< 0.001), schizophrenia (6.3[4.1-9.6], p< 0.001), ADHD (1.9[1.7-2.2], p< 0.001), PTSD (1.4[1.1-1.8], p=0.002), childhood abuse (15.7[5.5-44.6], p< 0.001). Whereas FD showed lesser association with GERD (0.72[0.7-0.74], p< 0.001) and constipation (0.8[0.7-0.9], p=0.001).
Discussion: We report a declining trend in primary FD hospitalizations over the last decade, possibly due to a better understanding of pathophysiology. IBS, smoking, substance abuse, schizophrenia, and childhood abuse showed a very strong association with FD hospitalizations.

Disclosures:
Rahul Pamarthy, MD1, Vaishnavi Boppana, MD2, Hassam Ali, MD3, Christopher Chang, MD, PhD4. P3369 - Trends of Functional Dyspepsia Hospitalizations and Prevalence of Psychiatric and Non-Psychiatric Co-Morbidities: A Decade-Long Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1East Carolina University, Greenville, NC; 2University of New Mexico, Albuquerque, NM; 3ECU Health Medical Center / Brody School of Medicine, Greenville, NC; 4University of New Mexico Health Sciences Center, Albuquerque, NM
Introduction: Functional dyspepsia (FD) has been strongly associated with common psychiatric conditions like anxiety, depression, and bipolar disorder and non-psychiatric conditions like GERD, IBS, and gastroparesis. We aim to study the trends of FD hospitalizations and their association with these disorders.
Methods: We conducted a retrospective study using the National Inpatient Sample (NIS) database, to analyze trends of hospitalizations with a primary diagnosis of FD and the prevalence of common psychiatric and non-psychiatric comorbidities in these hospitalizations from Jan 1, 2009, to Dec 31, 2019.
Results: There was a total of 37,237 weighted hospitalizations with a primary diagnosis of FD at the time of discharge. The trend of hospitalizations for FD declined from 4,900 (13 per 100,000 total NIS hospitalizations) in 2009 to 1,220 (3.4 per 100,000 total NIS hospitalizations) in 2019 (p< 0.001). Adjusted linear regression revealed a rising trend in the length of stay for FD patients from 3.3 days in 2009 to 5.3 days in 2019 (P< 0.001); and an increasing trend in mean inpatient charges from $23,827 in 2009 to $50,831 in 2019 (P< 0.001). Among FD hospitalizations, an increasing trend was observed in the prevalence of PUD history (p=0.049), GERD (p< 0.001), acute pancreatitis (p=0.0008), IBS (p=0.0005), gastroparesis (p=0.019), obesity (p< 0.001), depression (p< 0.001), bipolar disorder (p=0.03) and alcohol abuse (p=0.011). A decreased trend was noticed in constipation (p< 0.001) during FD hospitalizations. On adjusted regression analysis, FD was strongly associated with history of PUD (2.8[2.5-3.2], p< 0.001), acute pancreatitis (3.3[3-3.8], p< 0.001), IBS (5.2[4.6-5.8], p< 0.001), gastroparesis (1.6[1.5-1.7], p< 0.001), obesity (3.3[3-3.5], p< 0.001), smoking (6.8[6.4-7.3], p< 0.001), alcohol (2.8[2.4-3.2], p< 0.001), substance abuse (9.2[8-10.6], p< 0.001), anxiety (2.1[1.7-2.5], p< 0.001), depression (1.4[1.3-1.5], p< 0.001), bipolar disorder (4.3[3.9-4.9], p< 0.001), schizophrenia (6.3[4.1-9.6], p< 0.001), ADHD (1.9[1.7-2.2], p< 0.001), PTSD (1.4[1.1-1.8], p=0.002), childhood abuse (15.7[5.5-44.6], p< 0.001). Whereas FD showed lesser association with GERD (0.72[0.7-0.74], p< 0.001) and constipation (0.8[0.7-0.9], p=0.001).
Discussion: We report a declining trend in primary FD hospitalizations over the last decade, possibly due to a better understanding of pathophysiology. IBS, smoking, substance abuse, schizophrenia, and childhood abuse showed a very strong association with FD hospitalizations.

Figure: Trends of common psychiatric illnesses for functional dyspepsia hospitalizations from 2009 to 2019
Disclosures:
Rahul Pamarthy indicated no relevant financial relationships.
Vaishnavi Boppana indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Christopher Chang indicated no relevant financial relationships.
Rahul Pamarthy, MD1, Vaishnavi Boppana, MD2, Hassam Ali, MD3, Christopher Chang, MD, PhD4. P3369 - Trends of Functional Dyspepsia Hospitalizations and Prevalence of Psychiatric and Non-Psychiatric Co-Morbidities: A Decade-Long Nationwide Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
