Tuesday Poster Session
Category: Functional Bowel Disease
P3370 - Efficacy of Peppermint Oil in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Katia El Jurdi, MD, MSc
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Katia El Jurdi, MD, MSc, Nader Al Souky, MD, Stephanie J. Melquist, MD, MPH, Daly Al-Hadeethi, MD, William J.. Salyers, MD, MPH, Mohamad El Zein, MD
University of Kansas School of Medicine, Wichita, KS
Introduction: The estimated global prevalence of irritable bowel syndrome (IBS) is 10-15%. IBS carries a substantial negative impact on patients’ quality of life as well as a socioeconomic burden. Despite recent growth in the number of available therapeutic options, treatment remains challenging, leading to a growing interest in complementary and alternative medicine. Peppermint oil (PO) has recently become a potential treatment modality for IBS. The aim of this study is to investigate the efficacy and safety of PO in adult patients with IBS.
Methods: We systematically searched MEDLINE, Cochrane, EMBASE, and Web of Science for randomized controlled trials (RCT) of PO in adults with symptomatic IBS, published from inception through September 16, 2022. Eligible studies, satisfying the inclusion criteria, were appraised by the Cochrane risk of bias tool. We performed random-effects meta-analysis on the following outcomes: improvement in abdominal pain, improvement in the IBS score and IBS symptoms, as well as adverse events, including those leading to treatment discontinuation. Statistical analysis and forest plots comparing PO to placebo were done via Revman review manager.
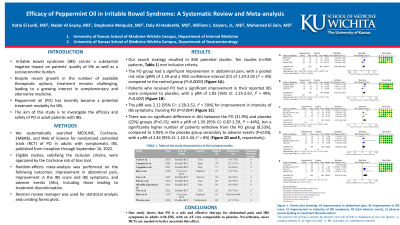
Results: Our initial search strategy resulted in a total of 836 potential studies. Of those, ten studies (n=956 patients, Table 1) met inclusion criteria. Patients in the PO group had a significant improvement in their abdominal pain, with a pooled risk ratio (RR) of 1.59, and a 95% confidence interval (CI) of 1.24-2.05 (I2 = 3%) compared to the control group (P=0.0003). Patients who received PO had a significant improvement in their reported IBS score compared to placebo, with a pooled RR of 1.83 [95% CI: 1.25-2.67, I2 = 49%, P=0.002]. The pooled risk ratio was 2.12 [95% CI: 1.28-3.52, I2 = 59%] for improvement in intensity of IBS symptoms, favoring PO (P=0.004). There was no significant difference in adverse events between the PO (31.9%) and placebo (22%) groups (P=0.15), with a pooled RR of 1.50 [95% CI: 0.87-2.59, I2 = 44%]. However, a significantly higher number of patients withdrew from the PO treatment group (8.53%), compared to 3.95% in the placebo group secondary to adverse events (P=0.03), with a pooled RR of 2.44 [95% CI: 1.10-5.44, I2 = 0%].
Discussion: Our study shows that PO is a safe and effective therapy for abdominal pain and IBS symptoms in adults with IBS, with an adverse event rate comparable to placebo. Nevertheless, more RCTs are needed to better ascertain this effect.

Disclosures:
Katia El Jurdi, MD, MSc, Nader Al Souky, MD, Stephanie J. Melquist, MD, MPH, Daly Al-Hadeethi, MD, William J.. Salyers, MD, MPH, Mohamad El Zein, MD. P3370 - Efficacy of Peppermint Oil in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kansas School of Medicine, Wichita, KS
Introduction: The estimated global prevalence of irritable bowel syndrome (IBS) is 10-15%. IBS carries a substantial negative impact on patients’ quality of life as well as a socioeconomic burden. Despite recent growth in the number of available therapeutic options, treatment remains challenging, leading to a growing interest in complementary and alternative medicine. Peppermint oil (PO) has recently become a potential treatment modality for IBS. The aim of this study is to investigate the efficacy and safety of PO in adult patients with IBS.
Methods: We systematically searched MEDLINE, Cochrane, EMBASE, and Web of Science for randomized controlled trials (RCT) of PO in adults with symptomatic IBS, published from inception through September 16, 2022. Eligible studies, satisfying the inclusion criteria, were appraised by the Cochrane risk of bias tool. We performed random-effects meta-analysis on the following outcomes: improvement in abdominal pain, improvement in the IBS score and IBS symptoms, as well as adverse events, including those leading to treatment discontinuation. Statistical analysis and forest plots comparing PO to placebo were done via Revman review manager.
Results: Our initial search strategy resulted in a total of 836 potential studies. Of those, ten studies (n=956 patients, Table 1) met inclusion criteria. Patients in the PO group had a significant improvement in their abdominal pain, with a pooled risk ratio (RR) of 1.59, and a 95% confidence interval (CI) of 1.24-2.05 (I2 = 3%) compared to the control group (P=0.0003). Patients who received PO had a significant improvement in their reported IBS score compared to placebo, with a pooled RR of 1.83 [95% CI: 1.25-2.67, I2 = 49%, P=0.002]. The pooled risk ratio was 2.12 [95% CI: 1.28-3.52, I2 = 59%] for improvement in intensity of IBS symptoms, favoring PO (P=0.004). There was no significant difference in adverse events between the PO (31.9%) and placebo (22%) groups (P=0.15), with a pooled RR of 1.50 [95% CI: 0.87-2.59, I2 = 44%]. However, a significantly higher number of patients withdrew from the PO treatment group (8.53%), compared to 3.95% in the placebo group secondary to adverse events (P=0.03), with a pooled RR of 2.44 [95% CI: 1.10-5.44, I2 = 0%].
Discussion: Our study shows that PO is a safe and effective therapy for abdominal pain and IBS symptoms in adults with IBS, with an adverse event rate comparable to placebo. Nevertheless, more RCTs are needed to better ascertain this effect.

Figure: Figure 1. Forest plot showing: A) improvement in abdominal pain, B) improvement in IBS score, C) improvement in intensity of IBS symptoms, D) total adverse events, E) adverse events leading to treatment discontinuation.
The overall risk of bias is shown by domain: the risk of bias is displayed as low risk (green, +), unclear (yellow,?), or high risk (red, −). RR: risk ratio, CI: confidence interval.
The overall risk of bias is shown by domain: the risk of bias is displayed as low risk (green, +), unclear (yellow,?), or high risk (red, −). RR: risk ratio, CI: confidence interval.
Disclosures:
Katia El Jurdi indicated no relevant financial relationships.
Nader Al Souky indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Mohamad El Zein indicated no relevant financial relationships.
Katia El Jurdi, MD, MSc, Nader Al Souky, MD, Stephanie J. Melquist, MD, MPH, Daly Al-Hadeethi, MD, William J.. Salyers, MD, MPH, Mohamad El Zein, MD. P3370 - Efficacy of Peppermint Oil in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
