Tuesday Poster Session
Category: Functional Bowel Disease
P3371 - Association of Ultra-Processed Food and Unprocessed or Minimally Processed Food Consumption With Bowel Function Among US Adults
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- CL
Chun-Han Lo, MD, MPH
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, NV
Presenting Author(s)
Chun-Han Lo, MD, MPH1, Longgang Zhao, PhD2, Euridice Martinez, PhD3, Chun-Wei Pan, MD4, Jeffrey Lee, MD, MPH5, Xuehong Zhang, PhD2, Harminder Singh, MD6, Niloy Samadder, MD7
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2Channing Division of Network Medicine and Harvard Medical School, Boston, MA; 3University of Sao Paulo, Sao Paulo, Sao Paulo, Brazil; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 6University of Manitoba, Winnipeg, MB, Canada; 7Mayo Clinic, Phoenix, AZ
Introduction: Ultra-processed food (UPF) consumption has increased over the past few decades, raising concerns about potential negative impact on the gut microbiome. The pro-inflammatory microenvironment induced by UPFs may lead to disordered bowel function but may be mitigated by increasing consumption of unprocessed or minimally processed foods (UMPs). In this study, we aimed to assess the association between UPF and UMP consumption and bowel function among US adults and the outcomes for substituting UPFs with UMPs.
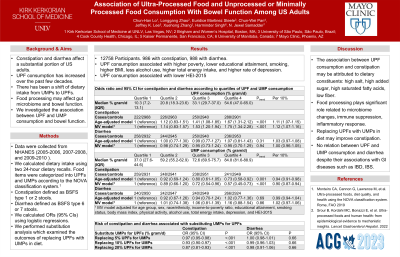
Methods: We performed a cross-sectional study using data from the National Health and Nutrition Examination Survey (2005-2010). Dietary intake was evaluated by two 24-hour dietary recalls. UPF and UMP intake (% of total gram/d) was derived based on the NOVA Classification. Constipation and diarrhea were defined according to Bristol Stool Form Scale. We used logistic regression to estimate the odds ratio (OR) and 95% confidence interval (CI) for constipation and diarrhea according to quartiles of UPF and UMP intake. Appropriate sample weights, stratification, and clustering were applied to account for the complex survey design. We performed substitution analysis to estimate the risk of constipation and diarrhea when replacing UPFs with an equivalent proportion of UMPs.
Results: Among 12,758 participants, there were 986 cases of constipation and 988 cases of diarrhea. The median UPF intake was 27% among total food intake in gram/d, while the median UMP intake was 66%. Participants who had greater UPF intake had higher risks of constipation (ORQ4 vs Q1, 1.87; 95% CI, 1.47-2.38) (Ptrend < 0.001) but not diarrhea (ORQ4 vs Q1, 0.95; 95% CI, 0.71-1.26) (Ptrend =0.99). Greater UMP intake was associated with a lower risk of constipation (ORQ4 vs Q1, 0.54; 95% CI, 0.43-0.69) (Ptrend < 0.001) but not diarrhea (ORQ4 vs Q1, 1.12; 95% CI, 0.85-1.48) (Ptrend =0.72). In addition, replacing 50% of UPF weight in diet with an equivalent proportion of UMPs was associated with a lower risk of constipation (OR, 0.68; 95% CI, 0.57-0.81).
Discussion: Dietary UPF intake was associated with a higher risk of constipation but not diarrhea, while UMP consumption had an inverse association with constipation. Substituting UPFs with UMPs may reduce the risk of constipation. These findings could be explained by differences in dietary constituents such as low fiber content in UPFs. Altered gut microbiota may also play a role through modulating the metabolic activities in colon.
Disclosures:
Chun-Han Lo, MD, MPH1, Longgang Zhao, PhD2, Euridice Martinez, PhD3, Chun-Wei Pan, MD4, Jeffrey Lee, MD, MPH5, Xuehong Zhang, PhD2, Harminder Singh, MD6, Niloy Samadder, MD7. P3371 - Association of Ultra-Processed Food and Unprocessed or Minimally Processed Food Consumption With Bowel Function Among US Adults, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2Channing Division of Network Medicine and Harvard Medical School, Boston, MA; 3University of Sao Paulo, Sao Paulo, Sao Paulo, Brazil; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 6University of Manitoba, Winnipeg, MB, Canada; 7Mayo Clinic, Phoenix, AZ
Introduction: Ultra-processed food (UPF) consumption has increased over the past few decades, raising concerns about potential negative impact on the gut microbiome. The pro-inflammatory microenvironment induced by UPFs may lead to disordered bowel function but may be mitigated by increasing consumption of unprocessed or minimally processed foods (UMPs). In this study, we aimed to assess the association between UPF and UMP consumption and bowel function among US adults and the outcomes for substituting UPFs with UMPs.
Methods: We performed a cross-sectional study using data from the National Health and Nutrition Examination Survey (2005-2010). Dietary intake was evaluated by two 24-hour dietary recalls. UPF and UMP intake (% of total gram/d) was derived based on the NOVA Classification. Constipation and diarrhea were defined according to Bristol Stool Form Scale. We used logistic regression to estimate the odds ratio (OR) and 95% confidence interval (CI) for constipation and diarrhea according to quartiles of UPF and UMP intake. Appropriate sample weights, stratification, and clustering were applied to account for the complex survey design. We performed substitution analysis to estimate the risk of constipation and diarrhea when replacing UPFs with an equivalent proportion of UMPs.
Results: Among 12,758 participants, there were 986 cases of constipation and 988 cases of diarrhea. The median UPF intake was 27% among total food intake in gram/d, while the median UMP intake was 66%. Participants who had greater UPF intake had higher risks of constipation (ORQ4 vs Q1, 1.87; 95% CI, 1.47-2.38) (Ptrend < 0.001) but not diarrhea (ORQ4 vs Q1, 0.95; 95% CI, 0.71-1.26) (Ptrend =0.99). Greater UMP intake was associated with a lower risk of constipation (ORQ4 vs Q1, 0.54; 95% CI, 0.43-0.69) (Ptrend < 0.001) but not diarrhea (ORQ4 vs Q1, 1.12; 95% CI, 0.85-1.48) (Ptrend =0.72). In addition, replacing 50% of UPF weight in diet with an equivalent proportion of UMPs was associated with a lower risk of constipation (OR, 0.68; 95% CI, 0.57-0.81).
Discussion: Dietary UPF intake was associated with a higher risk of constipation but not diarrhea, while UMP consumption had an inverse association with constipation. Substituting UPFs with UMPs may reduce the risk of constipation. These findings could be explained by differences in dietary constituents such as low fiber content in UPFs. Altered gut microbiota may also play a role through modulating the metabolic activities in colon.
Disclosures:
Chun-Han Lo indicated no relevant financial relationships.
Longgang Zhao indicated no relevant financial relationships.
Euridice Martinez indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Jeffrey Lee indicated no relevant financial relationships.
Xuehong Zhang indicated no relevant financial relationships.
Harminder Singh indicated no relevant financial relationships.
Niloy Samadder: Alimentiv Inc – Consultant. Jansen – Consultant. Recursion Pharmaceuticals – Consultant. Tempest Pharmaceuticals – Consultant.
Chun-Han Lo, MD, MPH1, Longgang Zhao, PhD2, Euridice Martinez, PhD3, Chun-Wei Pan, MD4, Jeffrey Lee, MD, MPH5, Xuehong Zhang, PhD2, Harminder Singh, MD6, Niloy Samadder, MD7. P3371 - Association of Ultra-Processed Food and Unprocessed or Minimally Processed Food Consumption With Bowel Function Among US Adults, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
