Tuesday Poster Session
Category: Functional Bowel Disease
P3377 - Fiber, Antispasmodics, and Laxatives Remain the Mainstay of IBS Treatment: A Potential Consequence of Weak Guideline Recommendations, Time Constraints, and High Drug Costs
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Samarth Shrivastava, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Samarth Shrivastava, MD, Neha Patel, MD
University of Texas Southwestern Medical Center, Dallas, TX
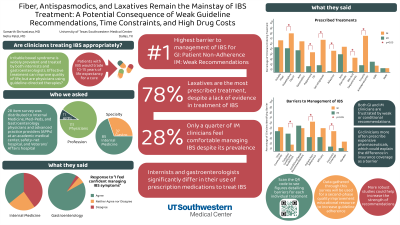
Introduction: Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction affecting 25% of the general population. Guidelines released by American College of Gastroenterology in 2021 and the American Gastroenterology Association in 2022 have several updated recommendations. Adherence to these guidelines ideally improves quality of life for patients suffering with IBS. In this study, we aimed to identify current practice patterns surrounding IBS management amongst physicians and Advanced Practice Providers (APPs).
Methods: Physicians and APPs practicing Gastroenterology (GI) and/or Internal Medicine (IM) at a large academic medical center, safety-net hospital and a Veterans Affairs health system were invited by email to complete an online survey consisting of 28 multiple-choice questions. The results of the survey will be used for a second-phase quality improvement educational resource to improve guideline adherence.
Results: 84 respondents completed the survey; 37% were gastroenterologists. 45 respondents (59.2%) agreed they feel comfortable managing IBS. In decreasing order, the barriers identified by participants regarding managing IBS were conditional or weak recommendations (n=45, 59.2%); time constraints (n=39, 51.3%); patient non-adherence (n=33, 43.4%), and drug efficacy (n=32, 42.1%). Over-the-counter laxatives were prescribed most frequently at 82.6% followed by antispasmodics (71.0%) and soluble fiber (69.6%). When asked about barriers to prescribing rifaximin and secretagogues, GIs reported high costs (78.6% and 67.9% respectively) and internists cited limited treatment experience (59.5% and 52.4% respectively). In regard to recommending psychotherapy, 86.1% of clinicians said they rarely or never referred patients to psychotherapy with wait time and lack of psychotherapists as the most common obstacles (65.3%).
Discussion: There are many areas for improvement in the treatment of patients with IBS. Barriers identified by clinicians suggest improving the strength of recommendations listed by the current guidelines. There is also an opportunity to provide education regarding the most efficacious treatments for IBS and which treatments are no longer recommended. Clinicians may particularly benefit from resources to help prescribe secretagogues and rifaximin and ways to improve high prescription drug costs. Tools to bridge the gap for psychotherapy as a treatment modality are desperately needed.
Disclosures:
Samarth Shrivastava, MD, Neha Patel, MD. P3377 - Fiber, Antispasmodics, and Laxatives Remain the Mainstay of IBS Treatment: A Potential Consequence of Weak Guideline Recommendations, Time Constraints, and High Drug Costs, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction affecting 25% of the general population. Guidelines released by American College of Gastroenterology in 2021 and the American Gastroenterology Association in 2022 have several updated recommendations. Adherence to these guidelines ideally improves quality of life for patients suffering with IBS. In this study, we aimed to identify current practice patterns surrounding IBS management amongst physicians and Advanced Practice Providers (APPs).
Methods: Physicians and APPs practicing Gastroenterology (GI) and/or Internal Medicine (IM) at a large academic medical center, safety-net hospital and a Veterans Affairs health system were invited by email to complete an online survey consisting of 28 multiple-choice questions. The results of the survey will be used for a second-phase quality improvement educational resource to improve guideline adherence.
Results: 84 respondents completed the survey; 37% were gastroenterologists. 45 respondents (59.2%) agreed they feel comfortable managing IBS. In decreasing order, the barriers identified by participants regarding managing IBS were conditional or weak recommendations (n=45, 59.2%); time constraints (n=39, 51.3%); patient non-adherence (n=33, 43.4%), and drug efficacy (n=32, 42.1%). Over-the-counter laxatives were prescribed most frequently at 82.6% followed by antispasmodics (71.0%) and soluble fiber (69.6%). When asked about barriers to prescribing rifaximin and secretagogues, GIs reported high costs (78.6% and 67.9% respectively) and internists cited limited treatment experience (59.5% and 52.4% respectively). In regard to recommending psychotherapy, 86.1% of clinicians said they rarely or never referred patients to psychotherapy with wait time and lack of psychotherapists as the most common obstacles (65.3%).
Discussion: There are many areas for improvement in the treatment of patients with IBS. Barriers identified by clinicians suggest improving the strength of recommendations listed by the current guidelines. There is also an opportunity to provide education regarding the most efficacious treatments for IBS and which treatments are no longer recommended. Clinicians may particularly benefit from resources to help prescribe secretagogues and rifaximin and ways to improve high prescription drug costs. Tools to bridge the gap for psychotherapy as a treatment modality are desperately needed.
Disclosures:
Samarth Shrivastava indicated no relevant financial relationships.
Neha Patel indicated no relevant financial relationships.
Samarth Shrivastava, MD, Neha Patel, MD. P3377 - Fiber, Antispasmodics, and Laxatives Remain the Mainstay of IBS Treatment: A Potential Consequence of Weak Guideline Recommendations, Time Constraints, and High Drug Costs, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
