Tuesday Poster Session
Category: Functional Bowel Disease
P3378 - Irritating to Diagnose? Irritable Bowel Syndrome Remains a Diagnosis of Exclusion
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Samarth Shrivastava, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Samarth Shrivastava, MD, Neha Patel, MD
University of Texas Southwestern Medical Center, Dallas, TX
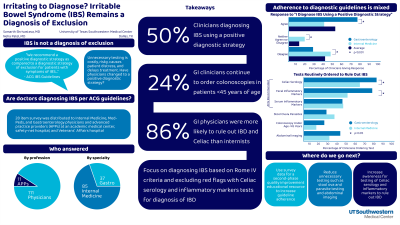
Introduction: Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction affecting around 25% of the population. Guidelines released by the American College of Gastroenterology (ACG) in 2021 urge a positive diagnostic strategy rather than a strategy of exclusion to diagnose IBS including ordering specific diagnostic tests. In this study, we aimed to identify attitudes and practice patterns surrounding the diagnosis of IBS among physicians and advanced practice providers (APPs).
Methods: Physicians and APPs practicing Gastroenterology (GI) and/or Internal Medicine (IM) at a large academic medical center, safety-net hospital and a Veterans Affairs health system were invited by email to complete an online survey consisting of 28 multiple-choice questions. The results of the survey will be used for a second-phase quality improvement (QI) educational resource to improve guideline adherence for diagnosis of IBS.
Results: 84 respondents completed the survey, 37% of whom were GIs. Interestingly, 38 respondents (48.7%) used a positive diagnostic strategy for IBS. Gastroenterologists were significantly more likely than IM physicians to use a positive diagnostic strategy (p=0.011). Serologic testing for celiac disease (83.3%) followed by fecal inflammatory markers (67.9%) and serum inflammatory markers (48.7%) were the most frequently ordered tests. Only 21% of respondents order colonoscopy in patients < 45 years of age to diagnose IBS. There was no statistically significant difference in the most common diagnostic tests ordered by IM physicians versus GIs.
Discussion: Our study finds several areas for quality improvement in the diagnosis of patients with IBS. Less than half of clinicians reported they used a positive diagnostic strategy for IBS suggesting there is need for better dissemination of the benefits of a positive diagnostic strategy as compared to a diagnostic strategy of exclusion. Almost 30% of gastroenterologists also stated they use a diagnostic strategy of exclusion. Additionally, more patients would benefit from testing for Celiac disease and inflammatory markers to capture Inflammatory Bowel Disease diagnoses. Finally, almost a third of respondents stated they routinely obtain stool Ova and parasite testing or imaging of the abdomen/pelvis to diagnose patients. Avoiding such unnecessary testing could significantly ameliorate the financial burden and the risks associated with unnecessary testing and procedures.
Disclosures:
Samarth Shrivastava, MD, Neha Patel, MD. P3378 - Irritating to Diagnose? Irritable Bowel Syndrome Remains a Diagnosis of Exclusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction affecting around 25% of the population. Guidelines released by the American College of Gastroenterology (ACG) in 2021 urge a positive diagnostic strategy rather than a strategy of exclusion to diagnose IBS including ordering specific diagnostic tests. In this study, we aimed to identify attitudes and practice patterns surrounding the diagnosis of IBS among physicians and advanced practice providers (APPs).
Methods: Physicians and APPs practicing Gastroenterology (GI) and/or Internal Medicine (IM) at a large academic medical center, safety-net hospital and a Veterans Affairs health system were invited by email to complete an online survey consisting of 28 multiple-choice questions. The results of the survey will be used for a second-phase quality improvement (QI) educational resource to improve guideline adherence for diagnosis of IBS.
Results: 84 respondents completed the survey, 37% of whom were GIs. Interestingly, 38 respondents (48.7%) used a positive diagnostic strategy for IBS. Gastroenterologists were significantly more likely than IM physicians to use a positive diagnostic strategy (p=0.011). Serologic testing for celiac disease (83.3%) followed by fecal inflammatory markers (67.9%) and serum inflammatory markers (48.7%) were the most frequently ordered tests. Only 21% of respondents order colonoscopy in patients < 45 years of age to diagnose IBS. There was no statistically significant difference in the most common diagnostic tests ordered by IM physicians versus GIs.
Discussion: Our study finds several areas for quality improvement in the diagnosis of patients with IBS. Less than half of clinicians reported they used a positive diagnostic strategy for IBS suggesting there is need for better dissemination of the benefits of a positive diagnostic strategy as compared to a diagnostic strategy of exclusion. Almost 30% of gastroenterologists also stated they use a diagnostic strategy of exclusion. Additionally, more patients would benefit from testing for Celiac disease and inflammatory markers to capture Inflammatory Bowel Disease diagnoses. Finally, almost a third of respondents stated they routinely obtain stool Ova and parasite testing or imaging of the abdomen/pelvis to diagnose patients. Avoiding such unnecessary testing could significantly ameliorate the financial burden and the risks associated with unnecessary testing and procedures.
Disclosures:
Samarth Shrivastava indicated no relevant financial relationships.
Neha Patel indicated no relevant financial relationships.
Samarth Shrivastava, MD, Neha Patel, MD. P3378 - Irritating to Diagnose? Irritable Bowel Syndrome Remains a Diagnosis of Exclusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
