Tuesday Poster Session
Category: General Endoscopy
P3407 - Role of Second-Look Endoscopy in Post-Endoscopic Submucosal Dissection and Post-Peptic Ulcer Bleeding Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Gowthami Sai Kogilathota Jagirdhar, MD
Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Gowthami Sai Kogilathota Jagirdhar, MD1, Jose Andres. Perez-Moscosco, MD2, Akshat Banga, MBBS3, Ruman Qasba, MBBS4, Saraswathi Lakkasani, MD5, Yatinder Bains, MD1
1Saint Michael's Medical Center, Newark, NJ; 2Saint Francis Health Systems, Tusla, OK; 3Sawai Man Singh Medical College, Jaipur, Rajasthan, India; 4Sher-i-kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India; 5Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction:
Gastrointestinal bleeding in post Endoscopic submucosal dissection (ESD) and in peptic ulcer disease (PUD) is commonly managed with endoscopic interventions. Recurrent bleeding following initial hemostasis in these conditions poses significant challenges, and second-look endoscopy (SLE) is often recommended even though its role is controversial. We, therefore, did a systematic review and meta-analysis to evaluate the effectiveness of SLE in ESD and PUD.
Methods: We searched through databases including Pubmed, Cochrane, and Embase from inception till Jan 2023, and included only randomized controlled trials comparing routine SLE Vs conservative management. PRISMA guidelines were followed and the protocol was registered with Prospero. The primary outcome of interest was recurrent GI bleeding for which a meta-analysis was performed using RevMan. Random effect models were used and the Mantel-Haenszel odds ratio was generated to describe the overall effect size.
Results:
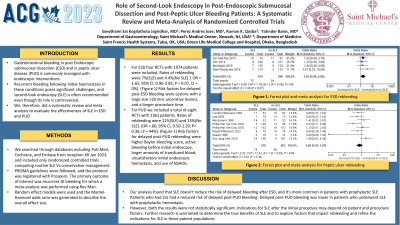
For ESD four RCTs with 1074 patients were included. Rates of rebleeding were 7%(SLE) and 4.4%(No SLE). ( OR = 1.65, 95% CI, 0.96-2.85; P = 0.07, I2 = 0%). (Figure 1) Risk factors for delayed post-ESD bleeding were Lesions with a large size >20 mm, ulcerative lesions, and a longer procedure time.
For PUD we included a total of eight RCTs with 1361 patients. Rates of rebleeding were 11%(SLE) and 13%(No SLE). (OR =.80, 95% CI, 0.50-1.29; P= 0.36, I2 = 44%). (Figure 1) Risk factors for delayed post-PUD rebleeding were higher Baylor bleeding score, active bleeding before initial endoscopy, larger amounts of transfused blood, unsatisfactory initial endoscopic hemostasis, and use of NSAIDs.
Discussion: Our meta-analysis suggests that SLE cannot reduce the risk of delayed bleeding post-ESD. Delayed bleeding was more common in patients who had prophylactic SLE than those who did not. Patients who had SLE had a reduced risk of delayed post-PUD bleeding. Delayed post-PUD bleeding was lower in patients who underwent SLE with prophylactic hemostasis. However, both the results were not statistically significant. Indications for Second-look endoscopy after the initial procedure may depend on patient and procedure factors. Further research is warranted to determine the true benefits of SLE and to explore factors that impact rebleeding and refine the indications for SLE in these patient populations.

Disclosures:
Gowthami Sai Kogilathota Jagirdhar, MD1, Jose Andres. Perez-Moscosco, MD2, Akshat Banga, MBBS3, Ruman Qasba, MBBS4, Saraswathi Lakkasani, MD5, Yatinder Bains, MD1. P3407 - Role of Second-Look Endoscopy in Post-Endoscopic Submucosal Dissection and Post-Peptic Ulcer Bleeding Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Michael's Medical Center, Newark, NJ; 2Saint Francis Health Systems, Tusla, OK; 3Sawai Man Singh Medical College, Jaipur, Rajasthan, India; 4Sher-i-kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India; 5Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction:
Gastrointestinal bleeding in post Endoscopic submucosal dissection (ESD) and in peptic ulcer disease (PUD) is commonly managed with endoscopic interventions. Recurrent bleeding following initial hemostasis in these conditions poses significant challenges, and second-look endoscopy (SLE) is often recommended even though its role is controversial. We, therefore, did a systematic review and meta-analysis to evaluate the effectiveness of SLE in ESD and PUD.
Methods: We searched through databases including Pubmed, Cochrane, and Embase from inception till Jan 2023, and included only randomized controlled trials comparing routine SLE Vs conservative management. PRISMA guidelines were followed and the protocol was registered with Prospero. The primary outcome of interest was recurrent GI bleeding for which a meta-analysis was performed using RevMan. Random effect models were used and the Mantel-Haenszel odds ratio was generated to describe the overall effect size.
Results:
For ESD four RCTs with 1074 patients were included. Rates of rebleeding were 7%(SLE) and 4.4%(No SLE). ( OR = 1.65, 95% CI, 0.96-2.85; P = 0.07, I2 = 0%). (Figure 1) Risk factors for delayed post-ESD bleeding were Lesions with a large size >20 mm, ulcerative lesions, and a longer procedure time.
For PUD we included a total of eight RCTs with 1361 patients. Rates of rebleeding were 11%(SLE) and 13%(No SLE). (OR =.80, 95% CI, 0.50-1.29; P= 0.36, I2 = 44%). (Figure 1) Risk factors for delayed post-PUD rebleeding were higher Baylor bleeding score, active bleeding before initial endoscopy, larger amounts of transfused blood, unsatisfactory initial endoscopic hemostasis, and use of NSAIDs.
Discussion: Our meta-analysis suggests that SLE cannot reduce the risk of delayed bleeding post-ESD. Delayed bleeding was more common in patients who had prophylactic SLE than those who did not. Patients who had SLE had a reduced risk of delayed post-PUD bleeding. Delayed post-PUD bleeding was lower in patients who underwent SLE with prophylactic hemostasis. However, both the results were not statistically significant. Indications for Second-look endoscopy after the initial procedure may depend on patient and procedure factors. Further research is warranted to determine the true benefits of SLE and to explore factors that impact rebleeding and refine the indications for SLE in these patient populations.

Figure: Figure 1 : Forest plot and meta-analysis for ESD rebleeding and Peptic ulcer rebleeding
Disclosures:
Gowthami Sai Kogilathota Jagirdhar indicated no relevant financial relationships.
Jose Perez-Moscosco indicated no relevant financial relationships.
Akshat Banga indicated no relevant financial relationships.
Ruman Qasba indicated no relevant financial relationships.
Saraswathi Lakkasani indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Gowthami Sai Kogilathota Jagirdhar, MD1, Jose Andres. Perez-Moscosco, MD2, Akshat Banga, MBBS3, Ruman Qasba, MBBS4, Saraswathi Lakkasani, MD5, Yatinder Bains, MD1. P3407 - Role of Second-Look Endoscopy in Post-Endoscopic Submucosal Dissection and Post-Peptic Ulcer Bleeding Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
