Tuesday Poster Session
Category: General Endoscopy
P3413 - The Stealthy Invader Unveiled: Duodenal Biopsy Discovers Strongyloides Stercoralis in an Immunosuppressed Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MK
Michelle H. Kwon, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Award: Presidential Poster Award
Michelle H. Kwon, MD1, Suvithan Rajadurai, MD1, Nathan Sairam, MD1, Jim ChunHao. Lee, MD, MPH2, Yousef Elfanagely, MD1, Ronan Farrell, MD3
1Warren Alpert Medical School of Brown University, Providence, RI; 2Rhode Island Hospital, Providence, RI; 3Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Strongyloidiasis, caused by the parasitic nematode Strongyloides stercoralis, can present with nonspecific gastrointestinal (GI) symptoms such as abdominal pain or weight loss. Immunosuppressed patients are at risk of disseminated strongyloidiasis which is often fatal thus early recognition is important. Here we present a case of a patient on chronic steroids experiencing odynophagia and weight loss, whose esophagogastroduodenoscopy (EGD) unexpectedly revealed Strongyloides.
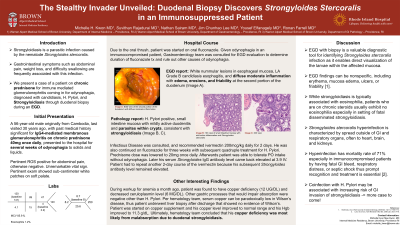
Case Description/Methods: A 56-year-old male who immigrated from Cambodia 30 years ago with history significant for IgG4-related membranous glomerulonephritis on chronic prednisone 40mg once daily presented to the hospital for several weeks for odynophagia. Labs showed signs of poor PO intake with weight loss, and elevated CRP of 34 with no leukocytosis or eosinophilia. Gastroenterology was consulted given odynophagia in an immunocompromised patient. EGD was performed and revealed white nummular lesions on the esophageal mucosa, consistent with candida esophagitis, along with diffuse moderate inflammation with edema, erosions and friability of the duodenum, which was biopsied (Image 1). Duodenal biopsy showed mildly active duodenitis and surprisingly, parasites within the crypts, consistent with strongyloidiasis (Image 2, 3). Infectious Disease was consulted and patient was started on ivermectin 200mcg/kg daily for 2 days, and prednisone dosage was lowered to 20mg once daily. After treatment, the patient was able to tolerate PO intake without odynophagia. Further chart review revealed elevated Strongyloides IgG antibody levels of 3.9. Patient was also found to have copper deficiency and it was presumed to be secondary to malabsorption from duodenal Strongyloides. Evaluations for Wilson’s disease with liver biopsy did not show copper toxicity.
Discussion: This case highlights the importance of considering strongyloidiasis in immunosuppressed patients presenting with nonspecific GI symptoms. While strongyloidiasis is typically associated with eosinophilia, patients on chronic steroids usually exhibit no eosinophilia, especially in the setting of fatal disseminated strongyloidiasis, thus timely recognition and treatment in this population is necessary. Endoscopic findings of strongyloidiasis such as erythema, mucosal edema, ulcers, or friability can be nonspecific, making biopsy a valuable diagnostic tool that enables direct visualization of the Strongyloides within the affected mucosa.

Disclosures:
Michelle H. Kwon, MD1, Suvithan Rajadurai, MD1, Nathan Sairam, MD1, Jim ChunHao. Lee, MD, MPH2, Yousef Elfanagely, MD1, Ronan Farrell, MD3. P3413 - The Stealthy Invader Unveiled: Duodenal Biopsy Discovers Strongyloides Stercoralis in an Immunosuppressed Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Michelle H. Kwon, MD1, Suvithan Rajadurai, MD1, Nathan Sairam, MD1, Jim ChunHao. Lee, MD, MPH2, Yousef Elfanagely, MD1, Ronan Farrell, MD3
1Warren Alpert Medical School of Brown University, Providence, RI; 2Rhode Island Hospital, Providence, RI; 3Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Strongyloidiasis, caused by the parasitic nematode Strongyloides stercoralis, can present with nonspecific gastrointestinal (GI) symptoms such as abdominal pain or weight loss. Immunosuppressed patients are at risk of disseminated strongyloidiasis which is often fatal thus early recognition is important. Here we present a case of a patient on chronic steroids experiencing odynophagia and weight loss, whose esophagogastroduodenoscopy (EGD) unexpectedly revealed Strongyloides.
Case Description/Methods: A 56-year-old male who immigrated from Cambodia 30 years ago with history significant for IgG4-related membranous glomerulonephritis on chronic prednisone 40mg once daily presented to the hospital for several weeks for odynophagia. Labs showed signs of poor PO intake with weight loss, and elevated CRP of 34 with no leukocytosis or eosinophilia. Gastroenterology was consulted given odynophagia in an immunocompromised patient. EGD was performed and revealed white nummular lesions on the esophageal mucosa, consistent with candida esophagitis, along with diffuse moderate inflammation with edema, erosions and friability of the duodenum, which was biopsied (Image 1). Duodenal biopsy showed mildly active duodenitis and surprisingly, parasites within the crypts, consistent with strongyloidiasis (Image 2, 3). Infectious Disease was consulted and patient was started on ivermectin 200mcg/kg daily for 2 days, and prednisone dosage was lowered to 20mg once daily. After treatment, the patient was able to tolerate PO intake without odynophagia. Further chart review revealed elevated Strongyloides IgG antibody levels of 3.9. Patient was also found to have copper deficiency and it was presumed to be secondary to malabsorption from duodenal Strongyloides. Evaluations for Wilson’s disease with liver biopsy did not show copper toxicity.
Discussion: This case highlights the importance of considering strongyloidiasis in immunosuppressed patients presenting with nonspecific GI symptoms. While strongyloidiasis is typically associated with eosinophilia, patients on chronic steroids usually exhibit no eosinophilia, especially in the setting of fatal disseminated strongyloidiasis, thus timely recognition and treatment in this population is necessary. Endoscopic findings of strongyloidiasis such as erythema, mucosal edema, ulcers, or friability can be nonspecific, making biopsy a valuable diagnostic tool that enables direct visualization of the Strongyloides within the affected mucosa.

Figure: Image 1: EGD view of the duodenum
Image 2: 10X view of the duodenum mucosa with mild active inflammation and worms consistent with Strongyloides stercoralis (black arrow)
Image 3: 20X view
Image 2: 10X view of the duodenum mucosa with mild active inflammation and worms consistent with Strongyloides stercoralis (black arrow)
Image 3: 20X view
Disclosures:
Michelle Kwon indicated no relevant financial relationships.
Suvithan Rajadurai indicated no relevant financial relationships.
Nathan Sairam indicated no relevant financial relationships.
Jim Lee indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Ronan Farrell indicated no relevant financial relationships.
Michelle H. Kwon, MD1, Suvithan Rajadurai, MD1, Nathan Sairam, MD1, Jim ChunHao. Lee, MD, MPH2, Yousef Elfanagely, MD1, Ronan Farrell, MD3. P3413 - The Stealthy Invader Unveiled: Duodenal Biopsy Discovers Strongyloides Stercoralis in an Immunosuppressed Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

