Tuesday Poster Session
Category: General Endoscopy
P3420 - Unusual Cause of Gastric Ulcerations in an Immunocompromised Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Muyi Li, MD
University of Washington
Seattle, WA
Presenting Author(s)
Muyi Li, MD1, Brian Mau, MD1, Joshua A. Lieberman, MD, PhD2, Anand Baxi, MD1
1University of Washington, Seattle, WA; 2University of Washington School of Medicine, Seattle, WA
Introduction: Syphilis has a wide range of manifestations depending on disease stage. Primary syphilis classically presents with painless genital ulceration, however in later stages the disease can spread to other parts of the body causing rash, liver and kidney injury, optic neuritis, and neurologic changes. While syphilis is well described in these other organ systems, gastric syphilis is rare and only occurs in 1% of all cases.
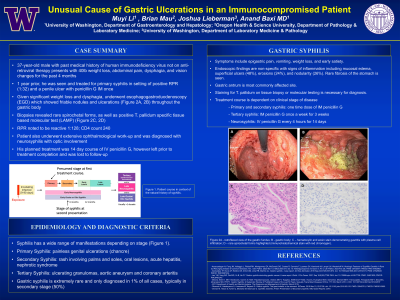
Case Description/Methods: A 37-year-old male with history of HIV not on treatment presented with weight loss, abdominal pain, dysphagia, and vision changes. His symptoms started 6 months ago, and ultimately led to a 40-pound weight loss over this time. His history was notable for treatment of gonorrhea, chlamydia, and syphilis infections a year ago. Labs on admission were notable for CD4 count 240, Treponema pallidum antibody reactive, and rapid plasma reagin (RPR) positive 1:128 concerning for active syphilis infection. Given the history of dysphagia with significant weight loss, he underwent esophagogastroduodenoscopy (EGD) which showed friable nodules and ulcerations (figure 1A, 1B) throughout the entire gastric body. Biopsies revealed rare spirochetal forms (figure 1D), as well as positive T. pallidum tissue-based Loop Mediated Amplification (LAMP). The patient also underwent extensive ophthalmological work-up and was diagnosed with neurosyphilis with optic involvement. He received penicillin for treatment of disseminated syphilis but left the hospital prior to completion of the treatment course.
Discussion: Diagnosis of gastric syphilis is challenging as symptoms can be vague including epigastric pain, nausea, weight loss, and early satiety. It typically develops after spirochetes spread through circulation and can often occur without other concurrent symptoms of infection. Endoscopic findings are non-specific with signs of inflammation including mucosal edema, superficial ulcers (48%), erosions (24%), and nodularity (26%). Gastric antrum is the most commonly affected site, but signs can also be seen throughout the gastric body. Staining for T-pallidum on tissue biopsy via immunofluorescence or nucleic acid amplification test (NAAT) is necessary for diagnosis. The treatment course is dependent on clinical stage of disease. Syphilis infection rates are rising in the United States, and given its non-specific clinical findings gastric syphilis requires a high degree of suspicion for diagnosis.

Disclosures:
Muyi Li, MD1, Brian Mau, MD1, Joshua A. Lieberman, MD, PhD2, Anand Baxi, MD1. P3420 - Unusual Cause of Gastric Ulcerations in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Washington, Seattle, WA; 2University of Washington School of Medicine, Seattle, WA
Introduction: Syphilis has a wide range of manifestations depending on disease stage. Primary syphilis classically presents with painless genital ulceration, however in later stages the disease can spread to other parts of the body causing rash, liver and kidney injury, optic neuritis, and neurologic changes. While syphilis is well described in these other organ systems, gastric syphilis is rare and only occurs in 1% of all cases.
Case Description/Methods: A 37-year-old male with history of HIV not on treatment presented with weight loss, abdominal pain, dysphagia, and vision changes. His symptoms started 6 months ago, and ultimately led to a 40-pound weight loss over this time. His history was notable for treatment of gonorrhea, chlamydia, and syphilis infections a year ago. Labs on admission were notable for CD4 count 240, Treponema pallidum antibody reactive, and rapid plasma reagin (RPR) positive 1:128 concerning for active syphilis infection. Given the history of dysphagia with significant weight loss, he underwent esophagogastroduodenoscopy (EGD) which showed friable nodules and ulcerations (figure 1A, 1B) throughout the entire gastric body. Biopsies revealed rare spirochetal forms (figure 1D), as well as positive T. pallidum tissue-based Loop Mediated Amplification (LAMP). The patient also underwent extensive ophthalmological work-up and was diagnosed with neurosyphilis with optic involvement. He received penicillin for treatment of disseminated syphilis but left the hospital prior to completion of the treatment course.
Discussion: Diagnosis of gastric syphilis is challenging as symptoms can be vague including epigastric pain, nausea, weight loss, and early satiety. It typically develops after spirochetes spread through circulation and can often occur without other concurrent symptoms of infection. Endoscopic findings are non-specific with signs of inflammation including mucosal edema, superficial ulcers (48%), erosions (24%), and nodularity (26%). Gastric antrum is the most commonly affected site, but signs can also be seen throughout the gastric body. Staining for T-pallidum on tissue biopsy via immunofluorescence or nucleic acid amplification test (NAAT) is necessary for diagnosis. The treatment course is dependent on clinical stage of disease. Syphilis infection rates are rising in the United States, and given its non-specific clinical findings gastric syphilis requires a high degree of suspicion for diagnosis.

Figure: Figure 1A - retroflexed view of the gastric fundus; B - gastric body; C – hematoxylin and eosin stain demonstrating gastritis with plasma cell infiltration; D – rare spirochetal forms highlighted (immunohistochemical stain with red chromogen).
Disclosures:
Muyi Li indicated no relevant financial relationships.
Brian Mau indicated no relevant financial relationships.
Joshua Lieberman indicated no relevant financial relationships.
Anand Baxi indicated no relevant financial relationships.
Muyi Li, MD1, Brian Mau, MD1, Joshua A. Lieberman, MD, PhD2, Anand Baxi, MD1. P3420 - Unusual Cause of Gastric Ulcerations in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
